Informacijos mokslai ISSN 1392-0561 eISSN 1392-1487
2020, vol. 87, pp. 86–99 DOI: https://doi.org/10.15388/Im.2020.87.28
Behaviour change interventions in breast and cervical cancer screening promotion
Vita Savicka
Riga Stradins University
vita.savicka@rsu.lv
Ingrīda Circene
Head doctor in MFD clinic
ingrida.circene@mfd.lv ; ingrida.circene@gamai.com
Summary. To encourage women to participate in breast and cervical state-paid screening programs, an experiment was conducted, during which easy access was provided to the screening and each woman who had not used the state-paid screening opportunity was addressed through direct communication. Screening coverage after the experiment improved up to 288%, demonstrating the importance of a behavioural economics nudge approach and tailored communication in the overall health communication process provided within the socio-ecological model.
Keywords: health communication, behaviour economics, behaviour change communication, social ecological model, breast and cervical cancer screening
Received: 30/10/19. Accepted: 02/03/20
Copyright © 2020 Vita Savicka, Ingrīda Circene. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Since 2009, the Ministry of Health and the National Health Service (NHS) of Latvia have provided a state-paid cancer early detection program providing a possibility to regularly ascertain the health condition and timely detect precancerous conditions or oncological diseases at early stage. Within the framework of this program, women aged 25 to 67 are sent an invitation to have a cervical cancer screening examination every three years, while women aged 50 to 68 are sent an invitation to have a breast cancer screening examination every two years. Examinations for these age groups are paid for by the state. Preventive breast examination is performed using the mammography method, while cervical cancer examination is performed by taking a cytological smear.
Every year, the National Health Service selects women aged 50, 52, 54, 56, 60, 62, 64, 66, 68 for mammography examinations and sends a letter of invitation for performance of examination paid for from the state budget. The letter is sent to the declared residence address and is valid two years. The state-funded cervical cancer preventive examination every three years is offered to every woman aged 25 to 70. Every three years, the NHS sends letters to women (25, 28, 31, 34, 37, 40, 43, 46, 49, 52, 55, 58, 61, 64, 67) to the declared residence address inviting them to come to the cervical cancer preventive examination. Having received the letter of invitation, the woman is invited to make an appointment in any medical institution performing the respective preventive examinations within the next three months. If the term is exceeded, the examination may be performed within two or three years, correspondingly, until the next letter of invitation is received. The letter specifies the medical institutions nearest to the place of residence, where the examination can be performed. However, the national program is little used – 65-70% of women do not attend the cervical cancer screening and 65% – the mammography screening (SPKC).
Objective – the objective of the article is to define the efficiency of using the behavioural economics nudge principle in the general communication process with target audiences.
A unique contribution of this article is that the experiment helps understand what tactics can be used in the health behaviour change, in order to promote performance of preventive examinations in female audience. The results mentioned in this article concern all women involved in the research.
Hypothesis. By using the nudge approach and involving additional medical personnel (a midwife) in communication with patients and examinations of the invited women, a higher coverage of the state-organized oncology screening can be achieved.
The research matters. Impact of the nudge approach and tailored communication on promotion of cancer screening efficiency.
Theory analysis
Achieving behaviour change is very difficult, because people’s habits and actions are determined by personal, social and external environment factors. The understanding of the role of communication in influencing people’s behaviour has changed dramatically since the 90s. Health communication researcher Renata Schiavo emphasizes that the behaviour change is based on behaviourism – the external environment plays a more important role in the behaviour change than internal factors (Schiavo, 2008). Public relations researcher James Grunig shares a similar view, stating that control over messages and the ability to influence people’s behaviour by communication has been an illusion rather than a reality (Grunig, 2009, 4). It underpins the strategic dimension of health communication, which involves research, communication and process management, achieving changes in the external environment that can contribute to the desired change in behaviour. The purpose of strategic communication is to expect actions, effects and behaviour change from the target audience (Schievio, 2008; Holmstorm 2015). When planning strategic communication, it should be borne in mind that change of the attitude does not always lead to desired changes in behaviour. For example, the strength of mass media campaigns is attraction of the target audience’s attention and influencing of social norms. However, for strategic communication to be effective, it must combine the power of the mass media with interpersonal interactions and community-based activities. By purposefully trying to only influence the behaviour of the individual, it can do more harm than good in the long run, as changing deep-seated behaviour is very difficult or even impossible; therefore, a holistic, preventive approach is necessary (Wood, 2016). Namely, communication should be combined with activities creating a better environment for the desired behaviour and facilitating the behaviour change. A wide range of environmental (political, institutional and societal) influences contribute to changing behaviour of the individual. A wide range of authors points out that a complex approach is necessary to achieve the behaviour change (French, Gordon 2015; Wood, 2016), providing the behaviour change communication across multiple levels of society and influencing mutual determinants (Dustin, 2010; Golden, 2012, Crawshaw, 2014; Golden 2015; Joseph, 2016).
A complex approach is characterized by a social ecological model as follows. “Its use provides a shift in thinking from focusing on a specific problem and solving it through a behavioural change campaign to comprehensive, preventive interventions at the population level” (Wood, 2016, 107-118). Speaking about screening programs, the state-paid preventive examinations are undoubtedly a significant external influencing factor, which significantly contributes to the ability of the target audiences to perform these examinations; however, it, as mentioned above, does not have sufficient impact.
The socio-ecological perspective underlying the socio-ecological model is not based on a single discipline or theory, but rather on a broad paradigm combining different fields of research, e. g., sociology, psychology and public health studies, analysing interactions of people, community and environment (Stokols, 1996). Thus, the socio-ecological perspective provides a possibility to understand the interaction between the individual and the environment in the system – both physical, social and interpersonal environment influences the individual’s or group’s emotions, cognitive processes and actions, and vice versa – reveals how emotions, cognitive processes and actions form the physical, social and interpersonal environment (Oishi and Graham, 2010).
The socio-ecological model was introduced as a conceptual model in the 70s, but was formulated in theory only in the 80s. The model was revised and improved by an American psychology researcher Urie Bronfenbrenner. A significant feature of socio-ecological systems is a dynamic and ever-changing relationship in response to internal and external pressures (Schlüter et al. 2014). They evolve holistically through the interaction of actors, institutions, and resources formed by certain socio-ecological settings (Holling and Gunderson, 2002). It is important that socio-ecological analysis puts more emphasis on the interaction between dynamic situations and personal factors, rather than focusing on environmental, biological or behavioural determinants affecting the well-being (Stokols, 1996).
The socio-ecological model aims to understand the impact of multifaceted and interactive persons and environmental factors determining a person’s behaviour. The model is most often used to identify the behavioural and organizationally significant elements that must be taken into account in health promotion. The socio-ecological model helps understand the factors influencing the behaviour and also provides guidance for successful behaviour change interventions. The United Nations International Children’s Fund has created a socio-ecological model that is used to implement strategic communication to improve the target audience’s health (UNICEF, 2015). The model includes five nested hierarchical levels: individual, interpersonal, community, organization, and policy level.
The first or individual level involves biological factors and experience affecting the individual. The second – Interpersonal – level researches formal and informal social links and social support systems having the potential to influence behaviour of the individual. The third, the community level, researches the conditions and environment, in which social relationships take place, and attempts to identify the features that influence a person’s behaviour. The focus is on relationships formed among organizations. The fourth, organization level, researches organizational or social institutes with rules and regulations affecting how and how well services are provided and the interests of the target group are defended. The fifth, the policy level, looks at the broader social factors contributing to creation of an environment, where the behaviour of the target audience is promoted or hindered. This level includes local or national level normative regulations and tax policies, resource allocation and other factors (UNICEF, 2015). UNICEF believes that combinations of measures at all levels of the social ecology model should be used to prevent and control public health problems. Based on a socio-ecological model, UNICEF implements the communication strategies aimed at the development of the society (Communication for Developments). It is a systematic, planned and evidence-based approach promoting positive and measurable behaviour and social environment changes (UNICEF, 2015) by activating activities at all levels of the socio-ecological model.
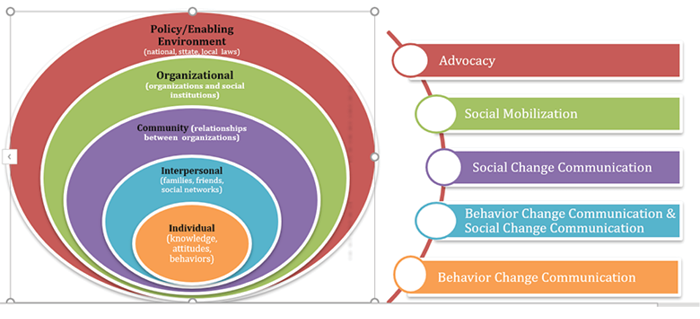
Table 1. UNICEF, 2015. “Communication for Development (C4D); MNCHN C4D Guide; Communication Strategy Guide for Maternal, Newborn, Child Health and Nutrition.” Access through Internet: https://www.unicef.org/cbsc/index_65738.html
As the most appropriate of strategies at the individual level is deemed the behaviour change communication, at the interpersonal level – the behaviour change and social change communication, at the community level – social change communication, at the organizational level – social mobilization, and at the policy level – advocacy (UNICEF, 2015). Applying a socio-ecological model is recommended in situations where it is necessary to encourage people to take more responsibility for their actions. The behaviour change impulses are transmitted both bottom-up and top-down, for example, peers create an example of good behaviour or policymakers create the conditions allowing to change behaviour of individuals positively (Lindridge et al., 2013).
Health communication researchers emphasize that application of the ecological model provides comprehensive and effective communication interventions (Berry, 2007; Golden, Earp 2012; Dutta – Bergman, 2005; Malikho, 2016, Glanz, Rimer, & Lewis, 2002; Wood, 2016).
The experiment reveals that interventions at the upper levels of the socio-ecological model (state-funded program, letters sent by institutions, communication campaigns) are not sufficient to ensure behaviour change. The role of the community and interpersonal level is also important in ensuring cooperation with GP practices, state institutions and in direct communication with women, who have not performed screenings. It is in this aspect of cooperation and actions that the effectiveness of both vertical and horizontal communication mix is demonstrated. At the same time, the experiment reveals the approaches used at the behaviour change communication level. None of the behaviour change models was used in the experiment, however, tailored communication combined with a behavioural economy nudge approach was applied. Tailoring has been defined as “any combination of strategies and information intended to reach one specific person, based on characteristics that are unique to that person, related to the outcome of interest, and derived from an individual assessment.” (Noar, 2011, 113). Traditionally, health communication is focused on a large audience, but this does not allow the individual aspects of the target audience – attitudes, self-esteem, self-efficiency, etc. – to be taken into account. “The basic premise behind tailored health communication is that information that is customized to an individual (rather than a group) will be viewed as more personally relevant, will be more likely to be read and cognitively processed, and ultimately will have a better chance of stimulating behavioural change” (Noar, 2011, 113).
The use of the tailored communication approach essentially overlaps with or can be complemented by behavioural economics approaches stimulating the individual by providing specific incentives for changing the individual behaviour or communicating messages that stimulate the behaviour of the target audience. Consequently, behavioural economics and tailored communication can be considered as a component of the behaviour change communication (BCC). It is often mentioned in the theoretical literature that health psychology models should be used in the BCC that reveal how people perceive their ability to change behaviour, social norms, barriers, threats, etc. The Health Believe Model (HBM) is offered for communication of screening programs as the basis for analysis. It was created in the middle of the last century, when, researching the effectiveness of tuberculosis screening programs, it was revealed that people were inactive in involvement in free tuberculosis (TB) health screening programs. The Health Belief Model was developed by social psychologists Hochbaum, Rosenstock and Kegel in 1950 (Malikhao, 2014). Behaviour stimulating and cognitive theory were integrated in this model (Skinner, Tiro, Champion 2015). The Health Belief Model is based on the belief that a person will perform health-related activities (such as screening) if they believe that it can prevent an adverse health condition and has a positive chance of avoiding adverse health conditions by implementing the recommended actions, and believe that they are able to successfully perform the recommended healthcare actions.
The researches have shown that, based on the Health Belief Model, assessing the needs of individuals and generating a consequential education and motivation can produce positive effects in cancer screening programs. Within the framework of one of the researches, women had to complete questionnaires assessing their health belief. The questionnaires were completed three times: before the start of the research, immediately after the intervention program and six months after the intervention. The results of the research showed that a specific intervention significantly improved women’s health belief and health behaviour, as nine out of ten women preformed a screening test within seven months after the end of the intervention program (Chania, Papagiannopoulou, Barbouni et al., 2013). Other researchers have also highlighted the usefulness of using the health belief model in analysis of perception, beliefs, as well as health benefits and barriers, in order to improve women’s participation in prevention screenings (Menon, Champion, Monahan, 2007).
The initial Health Belief Model consisted of four parts reflecting an individual’s perceived threats and benefits – perceived susceptibility/likelihood/sensitivity, perceived seriousness, perceived benefit and perceived barriers (Rosenstock, 1974). The authors offered specific concepts, in order to characterize the individual’s readiness to act. Later, in 1988, Rosenstock with co-authors supplemented this concept with the concept of self-efficacy.
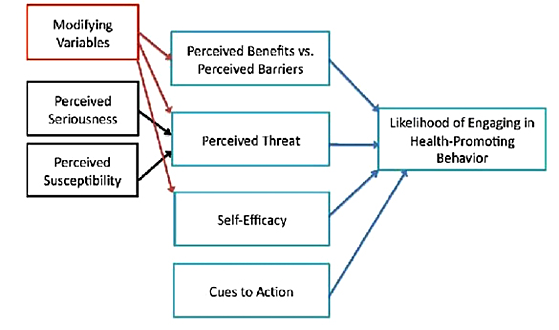
Table 2. Jones, Jensen, Scherr, Brown, Christy, Weave (2015) The Health Belief Model by Rosenstock, Strecher, and Becker (1988) Health Commun. 2015; 30(6): 566–576, https://doi.org/10.1080/10410236.2013.873363
As developers of the supplemented model emphasize, health belief model, social cognitive theory, self-efficacy, and locus of control have all been applied with varying success to problems of explaining, predicting, and influencing behaviour. Self-efficacy is proposed as a separate independent variable along with the traditional health belief variables of perceived susceptibility, severity, benefits, and barriers. Incentive to behave (health motivation) is also a component of the model. Locus of control is not included explicitly because it is believed to be incorporated within other elements of the model. (Rosenstock, Strecher, Becker, 1988)
According to Albert Bandura – self-efficacy is defined as people’s beliefs about their capabilities to produce designated levels of performance that exercise influence over events that affect their lives. Self-efficacy beliefs determine how people feel, think, motivate themselves and behave. Such beliefs produce these diverse effects through four major processes. They include cognitive, motivational, affective and selection processes to this theory, people who have high levels of self-efficacy tend to feel that they can perform very well at an activity and therefore attach more value to it. They do this through a process of first identifying a goal and then modifying their strategy and effort level to ensure that a goal is attained. (Bandura, 1994)
Bondura refers to the internal aspects helping change behaviour, mainly the experience of behaving. After people become convinced they have what it takes to succeed, they persevere in the face of adversity and quickly rebound from setbacks. The second way of creating and strengthening selfbeliefs of efficacy is through the vicarious experiences provided by social models. Seeing people similar to oneself succeed by sustained effort raises observers’ beliefs that they too possess the capabilities master comparable activities to succeed. Social persuasion is a third way of strengthening people’s beliefs that they have what it takes to succeed. People who are persuaded verbally that they possess the capabilities to master given activities are likely to mobilize greater effort and sustain it than if they harbour self-doubts and dwell on personal deficiencies when problems arise. (Bandura, 1994). Thus, it can be affirmed that self-efficacy can also be stimulated through direct communication, raising awareness that the perceived behaviour barriers are negligible and easy to overcome. Today, with the growing role of the behavioural economics, the concept of self-efficacy must be also supplemented with tailored communication and external stimuli directly targeted at the individual level.
Behavioural economics are known to attract attention to cognitive limitations, emotions (dislike of loss) (Thaler and Sunstein, 2008), as well as social norms (Ariely ,2008). However, Daniel Kahneman describes behavioural economics as a combination of intuitive beliefs, choices and reasoning. He, unlike other researchers, avoids the word rational. In his view, intuitive choices are impulsive, immediate, fast, easy, while reasoning is thoughtful, slow, effort-consuming and can correct errors caused by intuitive choices. Studies show that most choices are intuitive and only a few are based on reasoning or are corrected through reasoning (Etzioni 2011). Kahneman explains it not by poor reasoning of people, but by the choice to act intuitively. People’s behaviour is not governed by strict calculations, rather by what they experience and see at a given moment (Kahneman, 2003). Thus, it can be affirmed that irrational choices are people’s default mode (Etzioni, 2011). Other researchers believe that people act rationally, because they have used all the information available to them during making decisions (Etzioni, 2011), while Herbert Simon thinks that limited rationality is not irrationality, because people’s actions have an explanation (Simon, 1985).
D. Kahneman offers a concept of two-system thinking, where System 1 is more automated and consists of intuitive and emotional thinking, whereas System 2 is most often characterized by a person’s reflective and logical capacity. System 2, which is responsible for the person’s logical thinking, is most often taken into account in planning a society behaviour change (Ebert and Freibichler, 2017). Thus, nudge management has been developed that takes organizational context into account, in order to optimize people’s quick thinking and unconscious behaviour (Ebert and Freibichler, 2017). This means that by regulating a person’s choice architecture, while retaining a freedom of choice, we can contribute to the individual’s automatic decision-making, especially in the field of health and wellbeing (Ebert and Freibichler, 2017). If there are stimulating organizational conditions, a person is more likely to make a decision to change behaviour without analysing information or to accept that the behaviour will bring about a loss of having to give up something (Thaler and Sustein, 2009). Before making a choice, a person evaluates the risks cumulatively influencing the attitudes and values of individuals, groups of individuals, organizations. Risk assessment is influenced by social links – family, friends, associates, communities and social norms, as well as the information channels they listen to and the tone they give to perceived information (Etzioni, 2011).
There are several types of observations used to stimulate the desired health behaviour: default settings, where people most often use the opportunities given by the default mode, e. g., in the experiment, women were offered to choose several options, when to perform screening, but were not asked if they wanted to. It was taken into account in the experiment that people have limited time resources, therefore, the possibility to simplify choices and actions should be promoted. At the same time, it must be acknowledged that nudging is criticized for its short-term nature, because it does not affect people’s behaviour in the long term (Leigh, 2015).
Research
Method. Intervention study. Women who have not used the state-paid preventive examination possibility were directly addressed and offered to perform this preventive examination in a specific place (address) at a specific (convenient) time, allowing the respondent to change this time according to their capabilities. Women did not have to look for the letters of invitation sent by the state institution, as they were printed from the databases by the intervention study researchers.
Selection of participants. 6 GP practices located at one address were selected. So, all the women visiting these GP knew the location of this practice. Patients who had not performed the state-paid cervical cancer screening (aged 25-70) and women, who had not had a mammography screening within the last 2 years (aged 50-69), were chosen to be called from the pool of patients of the GP.
Course: For implementation of the intervention study, cooperation agreements were concluded with selected six GP practices, and a database of women invited to screening by the state institution (National Health Service) was used containing information on the number of letters sent to women registered in these six private practices in 2014, 2015 and 2016, total number of examined persons and a list of women, who have not used the service. In 2017, a pilot intervention study was conducted, during which, assessing women’s reactions, key messages were developed to be addressed to a woman when inviting her to a preventive examination. The intervention study ran from January 2018 to June 2018:
January 2018:
- 6 GP practices prepared a database of women to be invited with phone numbers;
- the call centre of the clinic uniting the GP practices was instructed to invite women to visit the midwife’s office by phone;
- information about the pilot project was posted on the clinic’s website and in social networks;
- information on the possibility to perform oncology screening examinations in the midwife’s office was placed at each of the 6 GP offices, as well as at the clinic reception desk, in the branches of the clinic;
- training of call centre employees was conducted on how to address women in the most effective way to use free oncology screening examinations.
February-March 2018:
- women were called. Those who did not pick up the phone also automatically received a text message about the opportunity to visit the midwife’s office and perform free examinations (29% of women who did not pick up the phone did not answer unknown callers, but called back having received the text message).
April-June 2018:
- repeated individual interviews were conducted with each of the GP, nurses, encouraging to address women to perform cervical screening and mammography examinations;
- information about the project was re-posted in social networks and on the clinic’s website.
Results
The obtained data show that in 2017, following the pilot intervention study and sending of the Latvian National Health Service’s invitation letters, inviting women to perform the cancer screening, the number of cervical cancer and breast cancer screenings in all 6 GP practices participating in the experiment increased by 20% to 288% compared to the previous year – 2016.
Having analysed the results of the pilot intervention study (2017) and the intervention study (2018), it can be concluded that both the pilot study and the study itself achieved remarkable results in screening growth, in some practices reaching even 100% completion. Statistical data showed growth in each of the GP practices within 25% to 40%.
Table 3. Increase of performed examination in GP practices before pilot intervention study (2016) and during pilot intervention study (2017) in amount and percentage.
|
Indicators |
May |
May |
June |
June |
July |
July |
August |
August |
|
Number of cytology examinations |
19 |
42 |
17 |
66 |
18 |
69 |
24 |
71 |
|
Number of mammography examinations |
14 |
20 |
19 |
35 |
12 |
31 |
16 |
32 |
|
Growth of cytology examinations (%) |
121% |
288% |
283% |
195% |
||||
|
Growth of mammography examinations (%) |
42% |
84% |
158% |
100% |
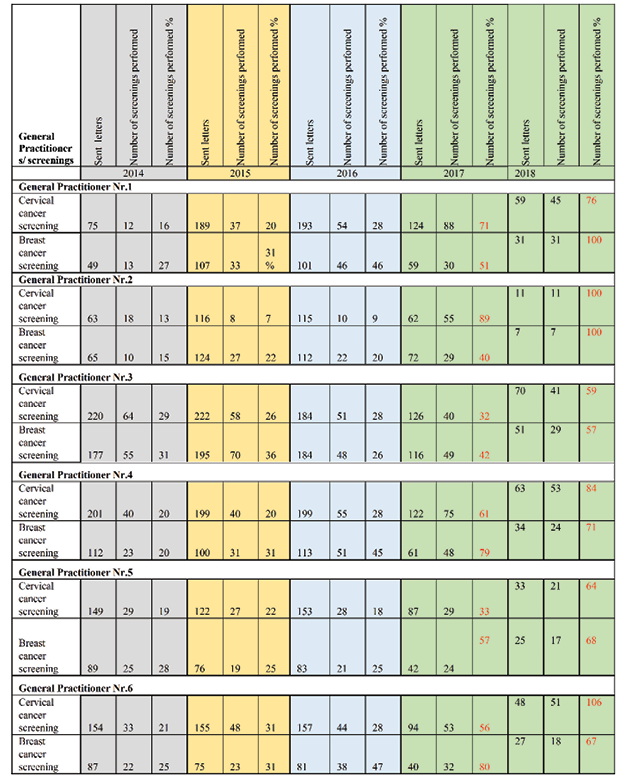
Table 4. Results or performed screenings in GP practices before the intervention study (2014-2016) and during the pilot intervention study (2017) and intervention study (2018).
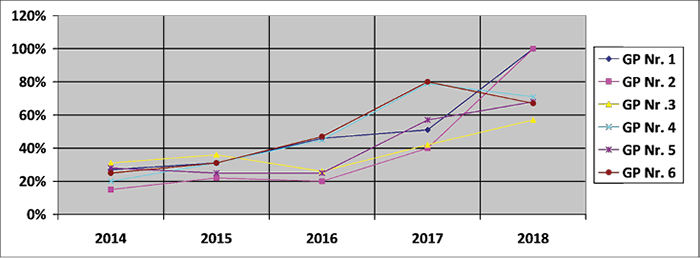
Table 5. Percentage increase of cervical cancer screening’s attendance in 6 GP practice before intervention study (2014-2016) and during pilot intervention study (2027) and intervention study (2018)
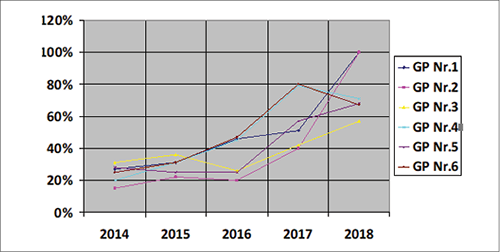
Table 6. Percentage increase of breast cancer screening’s attendance in 6 GP practices before intervention study (2014-2016) and during pilot intervention study (2017) and intervention study (2018)
In the first stage of the pilot project implementation, the growth of the results was faster, since the women invited within 3 years were identified.
Comparing the period when the women eligible for the National Surveillance Breast and Cervical Cancer Screening Program were sent invitation letters and the period when, in addition to the letters, the women received a midwife invitation call offering the screening to be made at a convenient time and in a place known to them – their GPs practice, when they had no need to search for the invitation letter received, the screening scope was significantly increased.
Conclusion and recommendations
Consequently, the hypothesis was confirmed, because by using the nudging approach and involving additional medical personnel (a midwife) in the examinations of the invited women, a significantly higher coverage of oncology screenings was achieved. Taking into account the local circumstances characterized by the heavy workload of GP, a significant incentive in the promotion of screening coverage had the additional average medical personnel performing screening functions, since women were able to choose the time they were most comfortable with for the screening. Therefore, changes at the policy level would be necessary, making this position with financing within the framework of the state-paid program. In order to promote the use of a state-paid service, it is necessary to involve a direct communicator, who communicates with the target group representatives (in the experiment it was a call centre), including the costs in the state-financed screening program. The fact that GP motivated women to participate in the oncology screening examinations by providing a comprehensive explanation served as a side factor. The intervention study demonstrates the need to use all levels of the socio-ecological model to achieve a significant progress in women performing cervical and breast cancer screenings. Activating the organization level (cooperation between state institutions and GP practices in information retrieval and analysis), as well as providing additional services creating changes at the interpersonal level, as well as at the individual level through BCC communication by using nudge and tailored communication approaches, can significantly improve screening coverage results. The nudge approach in the experiment involved both creating the additional convenience by providing a midwife’s services and direct communication including the default tactics. At the same time, the experiment does not reveal the direct effectiveness of the nudge approach; however, it confirms the view of the behavioural economics founders that the nudge approach can be used in combination with other communication interventions. Based on the recommendations to use HBM in promotion of screening programs also including an assessment of a person’s self-efficacy, it is recommended to promote self-efficacy through nudge and tailored communication approaches.
Literature
1. ARIELY, Dan (2008). Predictably irrational: The hidden forces that shape our decisions. New York: Harper Collins.
2. BANDURA, Albert (1994). Self-efficacy. In V. S. Ramachaudran (Ed.), Encyclopedia of humanbehavior (Vol. 4, pp. 71-81). New York: Academic Press. (Reprinted in H. Friedman[Ed.], Encyclopedia of mental health. San Diego: Academic Press, 1998).
3. BERRY, Diana (2007). Health Communication. Theory and practice. McGraw- Education.
4. BRONFENBRENNER, Urie (1977). “Toward an Experimental Ecology of Human-Development.” American Psychologist 32(7): 513-531. https://doi.org/10.1037/0003-066x.32.7.513.
5. CHANIA, M., PAPAGIANNOPOULOU, A., BARBOUNI, A. VAIDAKIS, D. ZACHOS, I. et al.(2013) Effectiveness of a Community-Based Health Education Intervention in Cervical Cancer Prevention in Greece, International Journal of Caring Sciences; Nicosia Vol. 6, Iss. 1, 2013: 59-68.5
6. CRAWSHAW, P. (2014). Changing Behaviours , Improving Outcomes Governing Healthy Lifestyles Through Social Marketing. 9, 1127–1139.
7. JONES Christina L. J, JENESN Jakob D., SCERRER Courtney L., BROWN Natasha R., CRISTY Katheryn and WEAVE Jeremy. (2015) The Health Belief Model as an Explanatory Framework in Communication Research: Exploring Parallel, Serial, and Moderated Mediation; Health Commun. 30(6): 566–576 https://doi.org/10.1080/10410236.2013.873363
8. DUSTIN, D. L., BRICKER, K. S., & SCHWAB, K. A. (2010). People and nature: Toward an ecological model of health promotion. Leisure Sciences, 32(1), 3–14. https://doi.org/10.1080/01490400903430772
9. DUTTA-BERGMAN, M. J. (2005). Theory and practice in health communication campaigns. Health Communication, 18(2), 103–122. https://doi.org/10.1207/s15327027hc1802_1
10. EBERT, Philip, FREIBICHLER Wolfgang (2017). “Nudge management: applying behavioural science to increase knowledge worker productivity”. Journal of organization Design 6 (4): 1-6. https://doi.org/10.1186/s41469-017-0014-1.
11. ETZIONI, Amitai (2011). “Behavioral Economics: Towar a New Paradigm.”American Behavioral Scientist 55(8): 1099–1119. https://doi.org/10.1177/0002764211412355.
12. GRUNING, James E. (2009). “Paradigms of global public relations in an age of digitalization.” PRismOnline PR Journal 6 (2): 1-19. Access through Internet: http://www.prismjournal.org/fileadmin/Praxis/Files/globalPR/GRUNIG.pdf.
13. GRUNING, James E.(2011). “Public relations and strategic management: Institutionalizing organization-public relationships in contemprorary society.” Central European Journal of Communication 4 (1): 11-31.
14. GOLDEN, S. D., & EARP, J. A. L. (2012). Social Ecological Approaches to Individuals and Their Contexts: Twenty Years of Health Education & Behavior Health Promotion Interventions. Health Education and Behavior, 39(3), 364–372. https://doi.org/ 10.1177/1090198111418634
15. GOLDEN, S. D., McLEROY, K. R., GREEN, L. W., EARP, J. A. L., & LIEBERMAN, L. D. (2015). Upending the Social Ecological Model to Guide Health Promotion Efforts Toward Policy and Environmental Change. Health Education and Behavior, 42(7440), 8–14. https://doi.org/10.1177/1090198115575098
16. NOIRIN, Hayes, O’TOOLE Leah, HALPENNY Ann Marie (2017). Introducing Bronfenbrenner: A Guide for Practitioners and Students in Early Years Education. New York: Routledge.
17. CRAWFORD Holling. S., un GUNDERSON Lance H.(2002). „Resilience and adaptive cycles.” No Panarchy: understanding transformations in human and natural systems. [b.v.]: Washington Island Press.
18. HOLMSTROM, Miranda (2015). “The Narrative And Social Media. Defence Strategic Communications.”The Offical Journal of the NATO Strategic Communications Centre of Excellence 1 (1): 118-132.
19. JEFF French, Gordon Ross (2015). Strategic Social Marketing. [b.v.]: Sage.
20. JOSEPH, R. P., DANIEL , C. L., THIND, H., & BENITEZ, T. J. (2016). Applying Psychological Theories to Promote Long-Term Maintenance of Health Behaviors. (Cld). https://doi.org/10.1177/1559827614554594
21. IlYES , Virág ( 2018). “Misbehaving: The Making of Behavioral Economics by Richard H. Thaler.” Corvinus Journal of Sociology and Social Policy 9 (1): 195-201. https://doi.org/10.14267/cjssp.2018.1.11.
22. LEIGH, Andrew (2015). “How behavioural economics does and can shape public policy.”The Economic and Labour Relations Review 26(2): 339-346. https://doi.org/10.1177/1035304615579346.
23. KAHNEMAN, Daniel (2003). “Maps of Bounded Rationality: Psychology for Behavioral Economics.” American Economics Review 93 (5): 1449-1475.
24. KAHNEMAN, Daniel (2012). Thinking, Fast and Slow. New York: Farrar, Straus and Giroux.
25. LINDRIDGE, Andrew, MacASKILL, Susan, GNICH, Wendy, EADIE, Douglas, HOLEM Ingrid (2013). “Applying an ecological model to social marketing communications.”European Journal of Marketing 47 (9): 1399-1420. https://doi.org/10.1108/ejm-10-2011-0561.
26. MALIKHAO, Patchanee (2014). Nova Science Publishers, Inc 6–7.
27. MALIKHAO, Patchanee (2016). Effective Health Communication for Sustainable Development, Hardback Public Health in the 21st Century English
28. MENON, U., CHAMPION, V., & MONAHAN , P. O. (2007). Health Belief Model Variables as Predictors of Progression in Stage of Mammography Adoption. 21(4), 255–261.
29. SENDHIL, Mullainathan, THALER Richard H. (2001). „Behavioral economics”.International Encyclopedia of Social Sciences 1: 1094-1100. doi:10.3386/w7948
30. SM, Noar, GRANT HARRINGTON, Nancy, VAN STEE, Stephanie, SHEMANSKI ALDICH, Rosalie (2011). Tailored Health Communication to Change Lifestyle Behaviors. American Journal of Lifestyle Medicine, 5(2), 112–122. https://doi.org/10.1177/1559827610387255
31. SCIAVO, Regina (2008). Health Communication: From Theory to Practice. In Journal of the Medical Library Association : JMLA (Vol. 96). https://doi.org/10.3163/1536-5050.96.1.72
32. SCHLUTER, Maja, HINKEL, Jochen, BOTS Pieter W. G., ARLINGHAUS Robert (2014). “Application of the SES framework for model-based analysis of the Dynamics of social-ecological systems.” Ecology and Society 19(1): 36. https://doi.org/10.5751/es-05782-190136.
33. SKINNER, C. S., Tiro, J., CHAMPION , V. L. (2015). The Health Belief Model. In K. Glanz, B. K. Rimer, & K. “V.” Viswanath (Eds.), Health behavior: Theory, research, and practice (pp. 75-94). San Francisco, CA, US: Jossey-Bass.
34. OISHI, Shigehiro, un JESSE Gra ham (2010). “Social Ecology: Lost and Found in Psychological Science”. Perspective on Psychological Science 5 (4): 356-377. https://doi.org/10.1177/1745691610374588.
35. ROSENSTOCK, Irwin M., STRECHER Victor J, BECKER Marshall H. (1988). Health Behavior and Health Education, The University of MichiganHealth Education Quarterly, Volume: 15 issue: 2,: 175-183. https://doi.org/10.1177/109019818801500203
36. SIMON, Herbert A (1985). “Human Nature in Politics: The Dialogue of Psychology with Political Science.” The American Political Science Review 79 (2): 293-304. https://doi.org/10.2307/1956650.
37. SPKC,Access through Internet: https://www.spkc.gov.lv/lv/tavai-veselibai/kampanas/rupes-par-veselibu-ir-gimenes-/
38. STOKOLS, Daniel (1996). “Translating Social Ecological Theory into Guidelines for Community Health Promotion.” American Journal of Health Promotion, 10 (4): 282-298.
39. THALER, Richard H., SUSTEIN Cass R. (2009). Nudge: Improving Decisions About Health, Wealth, and Happiness. New York: Penguin.
40. UNICEF (2015). “CommunicationforDevelopment (C4D); MNCHN C4D Guide; CommunicationStrategyGuideforMaternal, Newborn, Child Health and Nutrition.” Access through Internet: https://www.unicef.org/cbsc/index_65738.html
41. WOOD, Matthew (2016). “Social Marketing for Social Change.” Social Marketing Quarterly 22(2): 107-118. https://doi.org/10.1177/1524500416633429.