Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2020, vol. 19(1–2), pp. 27–33 DOI: https://doi.org/10.15388/LietChirur.2020.19.22
Video-assisted Treatment of Rectal Fistulas: the Experience and Treatment Results
Vitalii S. Groshilin
The Rostov State Medical University, Rostov-on-Don, Russia
E-mail vsgros@mail.ru
Viktoria G. Brizhak
The Rostov State Medical University, Rostov-on-Don, Russia
E-mail: vsgros@mail.ru
Evgeny Y. Khoronko
The Rostov State Medical University, Rostov-on-Don, Russia
E-mail: khoronko081@mail.ru
Petr V. Tsygankov
The Rostov State Medical University, Rostov-on-Don, Russia
E-mail: tsygankov_pv@rostgmu.ru
Yuri V. Khoronko
The Rostov State Medical University, Rostov-on-Don, Russia
E-mail: khoronko507@gmail.com
Abstract. Aim. Evaluation of the effectiveness and identification of the benefits of a video-assisted fistula treatment method using fistuloscopy, in comparison with traditional methods of surgical treatment of complex forms of chronic paraproctitis, trans- and extrasphincteric, relapsing rectal fistulas. Patients and methods. A complex analysis of the results of surgical treatment was carried out in 228 patients with chronic paraproctitis, transphincteric, ectrasphincteric, including recurrent rectal fistulas, divided into three groups (main and two control), depending on the surgical methods of chronic paraproctitis used. Results. The result of surgical treatment of pararectal fistulas in the three study groups was compared. The effectiveness of treatment was assessed by the results of immediate and long-term postoperative period. It has been established that the use of a video-assisted fistula treatment method using fistuloscopy excludes the presence of an extensive postoperative wound in the perianal region, which significantly reduces the likelihood of its secondary infection, and the sphincter trauma, and in fact virtually eliminates its insufficiency. The use of video-assisted method of treatment of fistulas made it possible to reduce the number of postoperative complications. Conclusion. The final results (92.7% of favorable outcomes) allow us to recommend a video-assisted treatment for fistulas for wide practical implementation.
Key words: perianal fistula, fistulaskopy, recurrent fistula, VAAFT.
Received: 2020/03/19. Accepted: 2020/04/30
Copyright © 2020 Vitalii S. Groshilin, Viktoria G. Brizhak, Evgeny Y. Khoronko, Petr V. Tsygankov, Yuri V. Khoronko. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Anorectal fistula is one of the most common diseases in coloproctology. According to the literature, rectal fistulas in the structure of coloproctological diseases range from 15% to 30% [1, 2]. More than 30% of patients with this pathology have complex forms of chronic paraproctitis. They are characterized by extrasphincter and high transsfincter location of the fistula, its branching, the presence of additional fistula passages and purulent cavities, as well as persistent recurrent course. Data from preventive examinations and treatment of patients with rectal fistulas indicate that up to 0.5% of people of working age suffer from this disease [2–4]. The high incidence of rectal fistulas can be explained not only by late treatment of patients with acute forms of paraproctitis for specialized care, but also by non-radical treatment of patients [5–7]. The presence of high transsfincter and extrasfincter fistulas of the rectum, complicated by the formation of infiltrative changes and purulent cavities in the pararectal spaces, is accompanied by a continuous course and frequent exacerbations of the inflammatory process [8]. Often this causes the occurrence and development of severe local changes that cause significant deformation of the anal canal and perineum, scar transformation of the anorectal locking apparatus muscles, resulting in insufficiency of the rectal locking apparatus, primarily the external sphincter. Unsuccessful outcomes of surgical treatment when attempting radical excision of fistulas are accompanied by significant trauma to the components of the external and internal sphincters after their intraoperative damage and replacement with scar tissue after wound healing. This is fraught (in addition to dysfunction of the pelvic elements) with the development of various degrees of fecal incontinence and flatus. According to modern authors [6, 7, 9], in patients with high transsfincter and extrasfincter fistulas of the rectum, the risk of anal incontinence up to 83% [1–3].
Another complication of chronic paraproctitis is pectenosis. These scar changes in the anal canal wall lead to a decrease in elasticity and scar narrowing, up to the formation of an anal stricture. In addition, the long-term course of the disease can lead to immunosuppression, a significant deterioration in the common condition of the patient and a decrease in the quality of life against the background of chronic purulent inflammation.
A radical method of treating patients with rectal fistulas only surgery is needed. To date, more than 100 methods of surgical treatment of patients with chronic paraproctitis and rectal fistulas have been published. The presence of a large number of known and newly proposed methods indicates that surgeons are dissatisfied with the results of treatment of complex trans-and extrasphincter rectal fistulas, as well as the lack of unified complex approaches to the choice of the operation method. Most authors state the need to improve the results of treatment of complicated forms of paraproctitis [1, 4, 8, 10]. The development of a differentiated algorithm for selecting a treatment method for chronic paraproctitis and justification of treatment methods for high complex complete extra- and transsphincter fistulas will significantly improve long-term results.
For recurrent high transsfincter and extrasfincter fistulas of the rectum, four main types of surgery are most often used in surgery: excision of the fistula, with suturing of its stump in the perineal wound with a posterior dosed sphincterotomy-the method of A. N. Ryzhikh (in two variants); excision of the fistula with plastic movement of the anal mucosa; excision of the fistula with suturing of the sphincter; excision of the fistula with ligature. Ligature method, excision of the fistula with suturing of the sphincter, as well as operations using the A. N. Ryzhikh method have a high risk of developing postoperative anal sphincter insufficiency with insufficient radicality and long-term treatment. After excision of the fistula with plastic displacement of the anal mucosa, there is a high probability of retraction or necrosis of the reduced area, due to a violation of microcirculation in the flap during the scarring process in the anal canal. In addition, if the displaced mucosal flap is not adequately spliced with the underlying scar-altered tissues of the anal canal wall, the risk of failure of the internal orifice plastic and, consequently, recurrence of the fistula increases. Pronounced scarring in the perianal region, multiple fistulas and purulent cavities, do not allow radical removal of pathologically altered tissues due to difficulties in closing the wound defect [1–3, 6, 9].
Therefore, the methods of surgical intervention described above do not provide for suitable closure and revascularization of the residual cavity, rectal wall, and wound defect.
Thus, the introduction of new effective surgical interventions in patients with rectal fistulas, especially with their recurrent course, is currently a very urgent task of surgery.
Aim
Evaluate the effectiveness and identify the advantages of video-assisted fistula treatment using fistuloscopy, in comparison with traditional methods of surgical treatment of complex forms of chronic paraproctitis, trans- and extrasphincter, recurrent rectal fistulas.
Patients and methods
In the surgical Department of the clinic of the Rostov State Medical University, 228 patients with chronic paraproctitis, transfincter, extrasphincter, including recurrent rectal fistulas, were treated in the period from 2012 to 2017. Of these, 156 are men (67.8%) and 72 are women (31.2%). The average age of men was 31.5±7.9 years, and the average age of women was 47.1±9.4 years. According to the duration of the disease, patients were distributed as follows: less than 6 months – 26 patients (11.4%), from 6 months to 1 year – 86 (37.7%), from 1 to 3 years – 46 (20.2%), from 3 to 5 years – 45 (19.7%), more than 5 years – 25 patients (11%). The criteria for exclusion from the study were: the presence of intrasfincter pararektal fistulas in patients; fistulas caused by specific diseases; rectal neoplasms (including patients who underwent radical surgery for cancer), inflammation bowel desease.
Patients with transfincter fistulas was 34 (14.9%), of them relapsing – 5 (2.2%), with extrasphincter fistulas of I degree of difficulty – 24 (10.5%), including relapsing – 6 (2.6%), extrasphincter fistulas of II stage of – 29 (12.7%), of them relapsing –6 (2.6%), extrasphincter fistulas of III stage – 96 (42.1%), of which recurrent fistulas – 17 (7.4%), extrasphincter fistulas IV stage – 45 (19.7%), of them relapsing – 11 (4.8%). 51 patients (22.4%) with a combined pathology of the anal canal that required simultaneous surgical correction. Chronic hemorrhoids of stage III–IV were detected in 21 patients (hemorrhoidectomy), chronic anal fissure in 27 patients (excision of the anal fissure, if necessary – anoplasty or dosed dilatation of the anal canal), adenomatous polyps of the anal canal – 3 observations (polypectomy).
The volume of surgical treatment was determined by the type of fistula and the duration of the disease and corresponded to the recommendations of the “Association of coloproctologists of Russia”, while the main group followed the principles of video-assisted anal fistula treatment (VAAFT, Carl Storz, Germany) for video-assisted treatment of complete rectal fistulas using fistuloscopy (Figure 1).
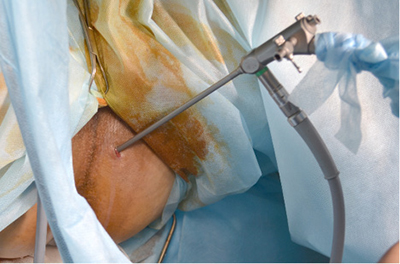
Figure 1. Video-assisted treatment using fistuloscopy
All 228 patients who met the study criteria were divided into three groups (the main group and two control groups), depending on the methods used for surgical treatment of chronic paraproctitis, complex trans- and extrasphinter, and recurrent rectal fistulas. The main group was formed of 55 patients (24.1%) who used a video-assisted method of fistula treatment using fistuloscopy, in the first control group – 89 patients (39.1%) underwent fistula excision with the elimination of the internal opening (Figure 2), suturing its stump in the perineal wound (including the method of Redheads), in the second control group – 84 patients (36.9%) performed radical fistula excision with segmental proctoplasty (moving the U-shaped full-layer mucosa flap of the rectum and its fixation in the anal canal).
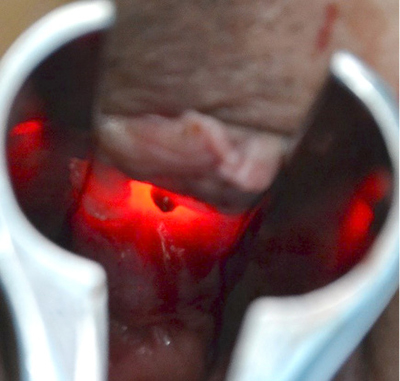
Figure 2. Elimination of the fistula
The effectiveness of treatment was evaluated based on the results of the immediate and long-term postoperative period. The results were evaluated as “good” with a stable recovery and no postoperative complications and no return of complaints. Clinical outcomes were considered “satisfactory” for certain complications that were completely treated conservatively, or when secondary sphincter weakness was detected (according to postoperative anorectal manometry) without any clinical manifestations of incontinence. Unsatisfactory results should include relapses of the disease that required repeated surgical treatment, as well as complications that are not compensated by conservative measures.
The postoperative monitoring period is 12 months.
Results
The results of treatment showed that the use of a video-assisted method using fistuloscopy, in addition to the treatment stage, has an important diagnostic value that influenced intraoperative tactics. Using fistuloscopy, it was possible to clearly topically identify the internal opening of the fistula, branches of the fistula and blindly ending residual cavities. The method allowed correcting preoperative diagnostic inaccuracies in the topography and complexity of the fistula course. The treatment stage, as the VAAFT method developed clinical experience, necessarily included electrocoagulation of the fistula canal, removal of necrotic tissues using a special pointed brush (Figure 3), stitching the internal opening of the fistula, and sealing the residual channel with bio-glue.
The table below shows the final postoperative distribution of patients by fistula complexity in the study groups (Table 1).
It should be noted that the use of video-assisted fistula treatment using fistuloscopy, which we used in the main group, excludes the presence of a large postoperative wound in the perianal area, which significantly reduces the likelihood of its secondary infection, and therefore virtually eliminates the occurrence of sphincter insufficiency. It is also important that there is no need for antibiotic therapy prescribed in the postoperative period. If in the control groups, antibacterial therapy was prescribed in all cases, in the main group, only 2 patients were treated when inflammatory changes appeared in the projection of the external fistula.
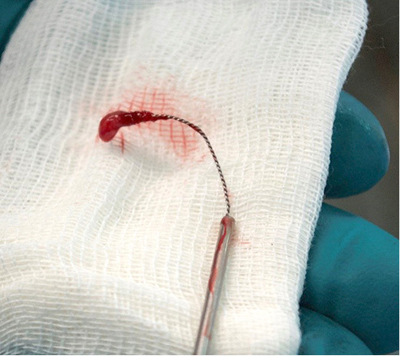
Figure 3. Removal of necrotic tissues using a special pointed brush
Table 1. Distribution of patients by the degree of fistula complexity in the study groups
|
Clinical groups Fistula in relation to the sphincter |
Basic group, n = 55 |
I test group, n = 89 |
II test group, n = 84 |
|
Transsphincteric fistula |
6 (10.9%), among them 2 recurrent |
16 (18%), among them 2 recurrent |
12 (14.3%), among them 1 recurrent |
|
Extrasphincteric fistula I stage |
6 (10.9%), among them 2 recurrent |
7 (7.9%), among them 2 recurrent |
11 (13.1%), among them 2 recurrent |
|
Extrasphincter fistula II stage |
7 (12.7%), among them 2 recurrent |
13 (14.6%), among them 2 recurrent |
9 (10.7%), among them 2 recurrent |
|
Extrasphincter fistula III stage |
23 (41.9%), among them 4 recurrent |
39 (43.8%), among them 8 recurrent |
34 (40.5%), among them 5 recurrent |
|
Extrasphincter fistula IV stage |
13 (23.6%), among them 3 recurrent |
14 (15.7%), among them 4 recurrent |
18 (21.4%), among them 4 recurrent |
|
Total recurrent fistula |
13 (23.6%) |
18 (20.2%) |
14 (16.7%) |
When analyzing the duration of administration of analgesics, the duration of hyperthermia, the timing of normalization of blood tests, postoperative bed days (5.23±2.4 in the main group, compared to 12.7±3.1 days in the first control group and 13.21±4.0 days in the second control group), the best results were obtained according to the interpreted criteria in the main group.
The results of treatment are indicative, taking into account all complications, including long-term periods. The total number of complications in the main group of clinical observations was 4 (7.3%), and in the first control group 30 (33.7%), in the second control group – 23 (27.4%). The proportion of complications, including those associated with subsequent recurrence of fistulas, was 4 (7.2%) in the main group. At the same time, 1 recurrent fistula later “closed” conservatively, in 3 cases, repeated surgical treatment in a hospital was required. The specific weight of complications is shown in the diagrams (Figure 4, A–C).
A 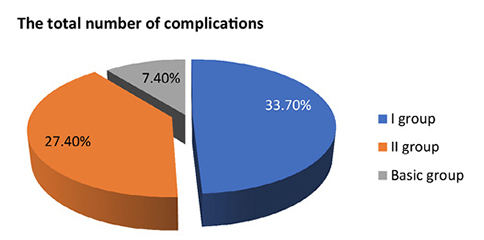
B 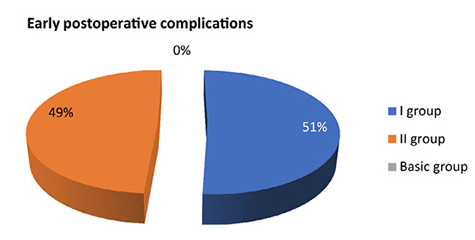
C 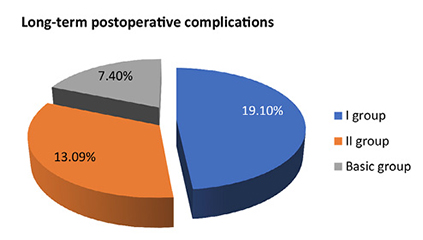
Figure 4. Proportion of postoperative complications (A), including early (B) and long-term complications (C)
In the first control group, the number of cases with complicated course of the postoperative period was 30 (33.7%), including 13 early postoperative complications (2 bleeding, 1 perianal abscess, 10 cases of inflammatory infiltrates and suppuration of surgical wounds) and 17 relapses and long-term complications (14 patients had a relapse of the disease that required repeated surgical treatment, in 3 cases there was an insufficiency of the anal sphincter, confirmed manometrically). In the second control group, 23 observations of complicated postoperative course (27.4%) were registered, including 12 early postoperative complications (1 patient had bleeding, 6 phenomena of retraction (or focal necrosis) of the reduced flap during proctoplasty, 5 observations – inflammatory infiltrates and suppuration of postoperative wounds that did not cause a relapse) and 11 long-term unsatisfactory outcomes (9 relapses of the disease that required repeated surgical treatment, in 2 cases there was insufficient anal sphincter I degree). As a result, good results were obtained in 51 patients of the main clinical group (92.7%), 59 patients of the first control group (66.3%), and 61 patients of the second control group (72.6%). Satisfactory, when complications were relieved – in 1 patient of the main group (1.8%), 13 patients of the first control group (14.6%) and 12 patients of the second control group (14.2%). The number of unsatisfactory results in the main group was 3 patients (5.5%), in the first control group was 17 (19.1%) patients and 11 patients (13.1%) – in the second control group.
Discussion
The use of video-assisted minimally invasive treatment (VAAPT) for complex and, especially, recurrent rectal fistulas has shown significant advantages over traditional methods, as evidenced by stable positive results with a minimum number of complications. The method confirmed high clinical efficacy with high safety achieved due to minimal trauma. In recurrent and complex extrasphincter fistulas, the risk of traumatic damage to previously discredited and often damaged components of the rectal occlusal apparatus is maximum, which creates a high probability of developing sphincter insufficiency and, as a consequence, urinary incontinence. In the main study group, using the VAAFT method, these complications were avoided by minimizing their risk.
Conclusions
The best long-term results were obtained in patients of the main group (92.7% – good, 1.8% – satisfactory, 5.5% – unsatisfactory) compared with results in the first control group (66.3% – good, 14.6% – satisfactory, 19.1% – unsatisfactory) and in the second control group (72.6% – good, 14.2% – satisfactory, 13.1% – unsatisfactory). These results were achieved in the main group, thanks to the use of modified VAAFT technology and fistuloscopy techniques, which significantly reduce the likelihood of early and late postoperative complications.
The presented data allow us to recommend a video-assisted method of fistula treatment using fistuloscopy for use in clinical practice in complex trans- and extrasphincter fistulas, as well as recurrent fistulas.
References
1. Ektov VN, Popov RV, Vollis YeA. Vozmozhnosti uluchsheniya rezul’tatov khirurgicheskogo lecheniya pryamokishechnykh svishchey s ispol’zovaniyem fibrinovogo kleya. Koloproktologiya 2013; 44(2): 44–50.
2. Song HK. New Techniques for Treating and Anal Fistula. J. Korean Soc. Coloproctol. 2012; 28(1): 7–12.
3. Frolov SA, Kuz’minov AM, Korolik VYu, Minbaev ShT, Bogormistrov IS, Chernozhukova MO. Metody lecheniya svishchej pryamoj kishki s primeneniem bioplasticheskih materialov. Koloproktologiya 2017; 3(61): 42a–43.
4. Malyugin AV, Malyugin VS, Linchenko VI, Halin DA. Sravnitel’naya ocenka hirurgicheskogo lecheniya ehkstrasfinkternyh svishchej pryamoj kishki. Medicinskij vestnik Severnogo Kavkaza 2013; 8(2): 34–36.
5. Slepykh NV, Il’kanich AYa. Fistuloskopiya pri lechenii svishchey pryamykh kishki. Koloproktologiya 2016; 2(46): 41.
6. Meinero P, Mori L. Video-assisted anal fistula treatment (VAAFT): a novel sphincter-saving procedure for treating complex anal fistulas. Techniques in Coloproctology 2011; 15(4): 417–422. DOI: 10.1007/s10151-011-0769-2.
7. Stazi A, Giarratano G, Mazzy M, Chini C. Sphincter-saving treatment of recurrent complex anal fistula with Video-Assisted Anal Fistula Treatment (VAAFT): a prospective study. Colorectal Disease 2014; 16(3): 4.
8. Groshilin VS, Sulanmuradov MI, Moskovchenko AN, Petrenko NA. Sovremennyye aspekty profilaktiki oslozhneniy posle obstruktivnykh rezektsiy distal’nykh otdelov tolstoy kishki. Fundamental’nyye issledovaniya 2013; 9(1): 24–27.
9. Gabibov SG, Shodiyev NA. Modifitsirovannyy videoassistirovannyy metod lecheniya svishchey pryamoy kishki. Koloproktologiya 2014; 3(49): 17–18.
10. Chivate SD. Commenton Meineroand Mori: Video-assisted anal fistulatreatment (VAAFT): anovel sphincter-saving procedure to repair complex anal fistulas. Tech Coloproctol. 2012; 16(6): 465–466. DOI: 10.1007/s10151-012-0873-y.