Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2020, vol. 19(1–2), pp. 34–41 DOI: https://doi.org/10.15388/LietChirur.2020.19.23
Complications after Laparoscopic Appendectomy for Complicated Appendicitis
Andrej Nikolovski
University Surgical Clinic “St. Naum Ohridski”, Skopje, North Macedonia
E-mail: andrejnikolovski@ymail.com
Shenol Tahir
University Surgical Clinic “St. Naum Ohridski”, Skopje, North Macedonia
E-mail: senol_tahir2002@yahoo.com
Dragoslav Mladenovikj
University Surgical Clinic “St. Naum Ohridski”, Skopje, North Macedonia
E-mail: dmladenovik@hotmail.com
Abstract. Background. Laparoscopic appendectomy is established method in the treatment of complicated appendicitis. Certain advantages of the technique do not fulfill the expectations for its superiority over the open appendectomy as when it is used for uncomplicated appendicitis. This is generally caused because of the high variety of postoperative complications reported in different series for complicated appendicitis. Material and methods. This prospective interventional clinical study analyzes 61 patients operated with laparoscopic and open appendectomy due to complicated appendicitis, with an end point of comparing the intra and postoperative complications in both groups. Results. Conversion in open appendectomy was forced in one patient (1.63%). The operative time was significantly shorter in the laparoscopic group (p = 0.048). Wound infection was significantly predominant in the open group (p = 0.045). Postoperative intraabdominal abscess occurred in one patient in the laparoscopic group (p = 0.52). The overall morbidity was 26.2% (7 patients in the laparoscopic, and 9 in the open group; p = 0.59). Length of stay was significantly shorter in the laparoscopic group (p = 0.00001). Conclusion. Certain significant advantages of the laparoscopic appendectomy as low incidence of wound infection, short hospitalization, less postoperative pain and faster socialization makes the laparoscopy up to date method in the treatment of complicated appendicitis.
Key words: complicated appendicitis, laparoscopic appendectomy, open appendectomy, complications.
Received: 2020/04/09. Accepted: 2020/04/28.
Copyright © 2020 Andrej Nikolovski, Shenol Tahir, Dragoslav Mladenovikj. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Acute appendicitis (AA) remains a diagnostic and therapeutic challenge as one of the most common abdominal emergencies with still imprecisely explained ethiopathogenesis [1]. The inflammatory appendicular process can subside with or without given antibiotic therapy [2, 3]. Otherwise, its progression can lead to an irreversible changes in the appendicular wall, finally resulting in perforation with all the following consequences [2]. At the same time, it represents the complicated form of acute appendicitis (complicated appendicitis – CA).
Complicated appendicitis is described as gangrenous appendicitis with or without macroscopically visible perforation or limited periappendicular abscess. In cases of free perforation, a diffuse secondary peritonitis can be present [1, 4].
More than 90% of AA cases are treated with surgery and the rate of use of laparoscopic appendectomy has surpassed the open method. In addition, a study that analyzes the data from the Nationwide Inpatient Sample (NIS) in the USA, in the period 2004–2011, shows continuous rising trend of laparoscopy usage. In 2004, it was used in 43.3%, while in 2011 the usage rose up to 75% of all performed appendectomies [5].
The complications associated with the procedure can be intra and postoperative. Unintentional bowel injury and bleeding are rare.
The postoperative ones can be graduated in minor and major complications. Most common minor postoperative complications are presented as sterile wound collections (seroma, hematoma), wound infection and paralytic ileus. Major complications, always expected and analyzed in the postoperative period, are bleeding, intraabdominal abscess (IAA), mechanical bowel obstruction, appendicular stump leak with stercoral fistula and laparotomy wound disruption (in open appendectomy) [6]. Some of them require additional intervention with or without general anesthesia. Rate of postoperative complications ranges between 3% and 28.7% [7].
A statistically significant higher rate of complications is reported (up to 35.5%) in cases of complicated appendicitis. Major factor is the complicated appendicitis itself [8]. Other analyzed risk factors for postoperative complications are female gender, ASA classification of 2 and more, age over 38.5 years and operative time more than 77 minutes [8, 9].
Objectives
This study assesses the postoperative complications in patients operated for complicated appendicitis with laparoscopic and open method.
Material and methods
Study design. This prospective interventional clinical study is conducted in our clinic in the period of 16 months. All patients or their parents signed the written informed consent for the procedure and for the study.
Patients. Sixty one patient with the age of 15 and more were included in the study in whom a complicated appendicitis was revealed during open and laparoscopic surgery. Grades of complications were: appendicular gangrene, appendicular perforation/rupture, periappendicular abscess and diffuse purulent peritonitis.
Operative techniques. One surgeon with mastered learning curve of more than 50 cases performed the laparoscopic procedure, and other two senior surgeons used the open method. For open appendectomy, McBurney and right pararectal incisions were used, while a standard tri port technique for the laparoscopic procedure (supraumbillical, suprapubic and left iliac fossa) was used. In cases of diffuse peritonitis a routine generous abdominal irrigation and suction was used. Abdominal drainage was not used routinely and it depended by the surgeons preference.
Perioperative interventions, treatment and follow up. Standard antibiotic prophylaxis was administered one hour prior the incision with 2 g of third generation Cephalosporine. Additional intraoperative 500 mg of Metronidazole was given intraoperatively. Both were continued in the next two postoperative days in doses of 2x2 g and 3x500 mg, respectively. Antithrombotic prophylaxis was conducted in all patients during the hospitalization period.
The postoperative follow up period duration was 30 days.
Statistics. A computer software SPSS for Windows v.23.0 was used for data analysis. Normality testing was done by using the Kolmogorov-Smirnov and Shapiro Wilk’s tests. Pearson Chi-square and Fisher exact test were used for qualitative data samples, while the Student t test and Mann-Whitney U test were used for quantitative data samples between the two groups. The values of p < 0.05 were taken as statistically significant.
Results
The patients were divided in two groups (laparoscopic-LA and open-OA). In terms of gender and age, the patients were presented as homogeneous groups. Male gender dominated in the two groups (65.6%, 62.1%, respectively; p = 0.77). Patients treated with laparoscopy were younger, with no significance (37.7±1.1 vs 42.8±16.2; p = 0.23). Both groups did not differ statistically in Leukocyte count (p = 0.66), CRP value (p = 0.54) and ASA classification (p = 0.12). Preoperative average values of Leukocytes were increased in both groups (15.9±3.9, 15.5±4.5, respectively). CRP presented with lower mean average values in the LA group without statistical significance (84.8 vs 92.8) (Table 1).
Table 1. Patient characteristics
|
Variable |
LA |
OA |
p |
|
Operated n |
n = 32 |
n = 29 |
|
|
Male n (%) |
21 (65.63) |
18 (62.07) |
X2 = 0.08 |
|
Female n (%) |
11 (34.4%) |
11 (37%) |
|
|
Age |
37.7±16.1 |
42.8±16.2 |
t = 1.22 |
|
Leukocyte |
15 940±3 955/mm3 |
15 465±4 550/mm3 |
t = 0.44 |
|
CRP |
111.69±89.6 |
126.02±93.9 |
Z = 0.6 |
|
ASA n (%) |
|
|
0.12 * |
X2 (Pearson Chi-square), t (Student t-tests), Z (Mann-Whitney test), *Fisher exact
The intraoperative finding was without statistical significance in both groups. Gangrenous appendicitis and diffuse peritonitis was more common in the LA group (15.75% and 13.8%, respectively; 28.1% and 20.7%, respectively), while perforation and periappendicular abscess were more common in the OA group (48.3% and 43.75%, respectively; 17.2% and 9.4%, respectively).
Conversion was done in one patient due to diffuse intraabdominal inflammatory process and technical inability to continue with laparoscopy in safe manner.
The results showed statistically significant difference in the operative time between the groups. The laparoscopic procedures were shorter (69.0±23.5 vs 79.4±15.6 min, p = 0.048).
There was no intra and postoperative mortality, and no cases of intraabdominal organ injury (Table 2).
Postoperative complications occurred in 16 patients (26.2%), 7 in LA and 9 in the OA group.
LA group had 5 minor and 2 major complications. Sterile wound collections (1 seroma and 2 port hematomas) occurred in 3 patients.
Two patients presented with postoperative pyrexia without the need of any additional intervention. There were no cases of wound infection. One patient was reoperated for early postoperative mechanical bowel obstruction and had uneventful postoperative period. One patient presented with postoperative IAA and it was successfully evacuated and drained by CT guidance (Figure 1).
Table 2. Intraoperative data
|
Variable |
LA |
OA |
p |
|
Intraoperative finding n (%) Gangrene |
6 (15.75) |
4 (13.79) |
0.73 * |
|
Operative time |
69.0 min±23.5 |
79.4 min±15.6 |
t = 2.02; p = 0.048 |
|
Conversion n (%) |
1 (1.63) |
/ |
/ |
X2 (Pearson Chi-square), t (Student t-tests), *Fisher exact
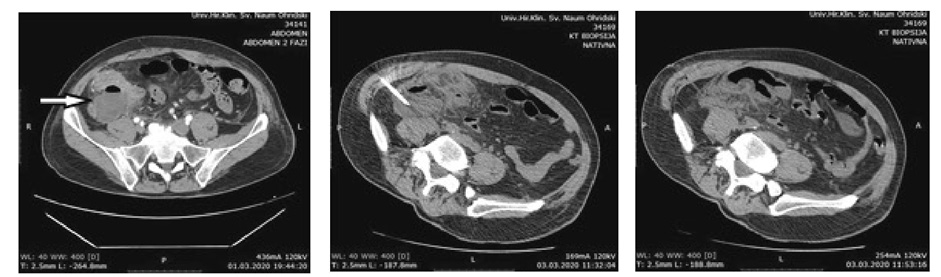
Figure 1. IAA evacuation and drainage
In the OA group there were 9 patients with complications (8 minor and 1 major). Wound seroma was noted in 2 patients, and wound infection occurred in 4 patients. One patient presented with allergic dermatitis. In one patient a stercoral fistula occurred and closed spontaneously without additional intervention.
The statistical difference in frequency of postoperative complications in the two groups was confirmed only for the wound infection (p = 0.045) in favor of the laparoscopic group.
Table 3. Postoperative data and complications
|
Variable |
LA |
OA |
p |
|
Seroma/hematoma n (%) |
3 (9.38) |
2 (6.9) |
0.55 * |
|
Wound infection n (%) |
0 |
4 (13.79) |
0.045 * |
|
Pyrexia n (%) |
2 |
1 |
1.0 * |
|
Alergic dermatitis n (%) |
0 |
1 (3.45) |
0.47 * |
|
Postoperative mechanical bowel obstruction n (%) |
1 |
0 |
0.52 * |
|
IAA (%) |
1 (3.13) |
0 |
0.52 * |
|
Stercoral fistula (%) |
0 |
1 (3.45%) |
0.47 * |
|
Operative reintervention n (%) |
1 (3.13) |
0 |
0.52 * |
|
Length of stay |
|
|
|
|
Readmissions |
1 (3.13) |
0 |
1.0 * |
|
Overall morbidity |
7 (21.8) |
9 (31.03) |
p = 0.59 * |
Z (Mann-Whitney test), *Fisher exact
Length of stay was statistically shorter in the LA group (p = 0.00001) with median length of stay of 4 days vs the open group with median length of stay of 6 days.
One patient in the LA group was readmitted.
Discussion
Certain advantages of the laparoscopic technique do not fulfill the expectations for its superiority over the open appendectomy as when it is used for uncomplicated appendicitis. There are still controversies and unanswered questions regarding the incidence of postoperative complications when laparoscopy is compared with the open appendectomy for the treatment of CA. Special emphasis is placed on the incidence of major complications, especially the IAA.
At it is written in the introduction of this study, the complication rate after appendectomy for complicated appendicitis can be as high as 35.5%.
Postoperative complication occurrence is associated with the intraoperative finding, in this case, the difficult finding of complicated appendicitis. It is a significant risk-factor for postoperative complications by itself [9].
One of the first studies for the laparoscopic treatment of CA is published in 2001 [10], while the first prospective study that reveals a positive trend of feasibility of laparoscopy is published in 2006 [11].
The latest relevant medical publications confirm that the laparoscopic appendectomy has determined its place in the treatment of CA as a modern and safe method. It represents serious competitor to the open method all around the world.
The severity of the inflammatory process can prolong the operative time in LA especially when an additional adhesiolysis, partial resection of great omentum, irrigation and suction of the abdominal cavity are required. Manipulation of the patient’s position, which can cause difficulties in proper positioning of the laparoscopic instruments, is often required [12].
Regardless of the intraoperative finding, the surgeons experience and the technical capabilities are important factor that has an impact on the operative time. Mastering the learning curve for LA reduces the operative time [12, 13]. This study showed statistically significant shorter operative time in the laparoscopic group.
The conversion rate for laparoscopic appendectomy ranges between 0% and 47% [14–18]. Factors associated with the risk for conversion are: comorbidity presence, retrocecal position of the appendix, diffuse peritonitis and appendicular abscess [19–22]. In this study, one conversion was done due to the severity of the inflammatory process.
Laparoscopy results with statistically significant lower rate of wound infection when compared with the open technique, regardless of the severity of the intraoperative finding [12, 14–16, 23, 24]. Our series, as expected, showed that the wound infections were more often present in the OA group with statistical significance.
Intraabdominal abscess occurrence is a serious postoperative complication that requires adequate treatment (sometimes a surgical one). Different series show heterogeneous data about its rate when compared between LA and OA [12, 16, 25–28]. Certain attempts are made in order to reduce its incidence such as reduction of the pneumoperitoneum pressure (low intraabdominal pressure) for eventual positive impact on bacterial translocation in the bloodstream [29, 30]. Further, pus collection suction with complete adhesiolysis and generous intraabdominal lavage with multiple drains are proposed [28]. Other authors suggest that intraabdominal lavage rises the incidence of IAA so they recommend only pus collection suction [12, 31, 32]. A third party series showed no difference between irrigation and suction versus suction alone that affects the IAA formation [33–35]. In our study, we used generous irrigation and suction and also a mandatory adhesiolysis. Intraabdominal drainage was used always in cases of diffuse peritonitis and periapendicular abscess, while in the rest of the cases, the indication for drainage was relative. There was one case of IAA in the LA group, which was statistically with no significance.
The IAA treatment can be operative (laparotomy) or with US or CT-guided percutaneous drainage. The minimal invasiveness of the procedure, its efficiency (over 90% successfulness) and no need for general anesthesia, makes the percutaneous drainage first choice method for post appendectomy IAA. However, it has some limitations when a diffuse interintestinal collections are present [36–38].
The length of stay in the LA group was significantly shorter. Most of the published comparative series, meta-analyses and reviews also show a statistically significant shorter length of stay when compared with the open appendectomy [12, 26, 39–45].
Conclusion
Laparoscopic appendectomy is established method in the treatment of complicated appendicitis, as a safe alternative to the open appendectomy. Some of the surgeons still have doubts about its quality and advantages over the open method. It is probably due to the heterogeneity of the reports that focus on the postoperative major complications. Still, the statistical significance of the low rates of wound infections, shorter length of stay, lesser postoperative pain, better cosmetic results, faster recovery and socialization make the laparoscopy always the current method in the treatment of CA, and also popular for scientific research.
References
1. D’Souza N, Nugent K. Appendicitis. Am Fam Physician. 2016; 93(2): 142–143.
2. Migraine S, Atri M, Bret PM, Lough JO, Hinchey JE. Spontaneously resolving acute appendicitis: clinical and sonographic documentation. Radiology 1997; 205(1): 55–58.
3. Cobben LP, de Van Otterloo AM, Puylaert JB. Spontaneously resolving appendicitis: frequency and natural history in 60 patients. Radiology 2000; 215(2): 349–352.
4. Petroianu A, Villar Barroso TV. Pathophysiology of Acute Appendicitis. JSM Gastroenterol Hepatol 2016; 4(3): 1062.
5. Masoomi H, Nguyen NT, Dolich MO, Mills S, Carmichael JC, Stamos MJ. Laparoscopic appendectomy trends and outcomes in the United States: data from the Nationwide Inpatient Sample (NIS), 2004–2011. Am Surg 2014; 80(10): 1074–1077.
6. Biondi A, Di Stefano C, Ferrara F, Bellia A, Vacante M, Piazza L. Laparoscopic versus open appendectomy: a retrospective cohort study assessing outcomes and cost-effectiveness. World Journal of Emergency Surgery 2016; 11(1): 44.
7. Sartelli M, Baiocchi GL, Di Saverio S, Ferrara F, Labricciosa FM, et al. Prospective Observational Study on acute Appendicitis Worldwide (POSAW). World Journal of Emergency Surgery 2018; 13: 19.
8. Patel SV, Nanji S, Brogly SB, Lajkosz K, Groome PA, Merchant S. High complication rate among patients undergoing appendectomy in Ontario: a population-based retrospective cohort study. Can J Surg. 2018; 61(6): 412–417.
9. Moreira LF, Garbin HI, Da-Natividade GR, Silveira BV, Xavier TV. Predicting factors of postoperative complications in appendectomies. Rev. Col. Bras. Cir. 2018; 45(5): e19.
10. Wullstein C, Barkhausen S, Gross E. Results of laparoscopic vs. conventional appendectomy in complicated appendicitis. Dis Colon Rectum 2001; 44(11): 1700–1705.
11. Towfigh S, Chen F, Mason R, Katkhouda N, Chan L, Berne T. Laparoscopic appendectomy signifcantly reduces length of stay for perforated appendicitis. Surg Endosc 2006; 20(3): 495–499.
12. Horvath P, Lange J, Bachmann R, Struller F, Konigsrainer A, Zdichavsky M. Comparison of clinical outcome of laparoscopic versus open appendectomy for complicated appendicitis. Surg Endosc 2017; 31(1): 199–205.
13. Yu MC, Feng YJ, Wang W, Fan W, Cheng HT, Xu J. Is laparoscopic appendectomy feasible for complicated appendicitis? A systematic review and meta-analysis. Int J Surg 2017; 40: 187–197.
14. Fukami Y, Hasegawa H, Sakamoto E, Komatsu S, Hiromatsu T. Value of laparoscopic appendectomy in perforated appendicitis. World J Surg 2007; 31(1): 93–97.
15. Katsuno G, Nagakari K, Yoshikawa S, Sugiyama K, Fukunaga M. Laparoscopic appendectomy for complicated appendicitis: a comparison with open appendectomy. World J Surg 2009; 33(2): 208–214.
16. Lim SG, Ahn EJ, Kim SY, Chung IY, Park JM, Park SH, Choi KW. A clinical comparison of laparoscopic versus open appendectomy for complicated appendicitis. J Korean Soc Coloproctol. 2011; 27(6): 293–297.
17. Stoltzing H, Thon K. Perforated appendicitis: is laparoscopic operation advisable? Dig Surg 2000; 17(6): 610–616.
18. Sauerland S, Jaschinski T, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev 2010; 6(10): 001546.
19. Antonacci N, Ricci C, Taffurelli G, Monari F, Del Governatore M, Caira A, Leone A, Cervellera M, Minni F, Cola B. Laparoscopic appendectomy: Which factors are predictors of conversion? A high-volume prospective cohort study. International Journal of Surgery 2015; 21: 103–107.
20. Liu SI, Siewert B, Raptopoulos V, Hodin RA. Factors associated with conversion to laparotomy in patients undergoing laparoscopic appendectomy. J Am Coll Surg. 2002; 194(3): 298–305.
21. Wagner PL, Eachempati SR, Aronova A, Hydo LJ, Pieracci FM, Bartholdi M, Umunna BP, Shou J, Barie PS. Contemporary predictors of conversion from laparoscopic to open appendectomy. Surg Infect (Larchmt) 2011; 12(4): 261–266.
22. Hellberg A, Rudberg C, Enochsson L, Gudbjartsson T, Wenner J, Kullman E, Fenyö G, Ringqvist I, Sörensen S. Conversion from laparoscopic to open appendicectomy: a possible drawback of the laparoscopic technique? Eur J Surg. 2001; 167(3): 209–213.
23. Garg CP, Vaidya BB, Chengalath MM. Eficacy of laparoscopy in complicated appendicitis. Int J Surg 2009; 7(3): 250–252.
24. Markides G, Subar D, Riyad K. Laparoscopic versus open appendectomy in adults with complicated appendicitis: systematic review and meta-analysis. World J Surg 2010; 34(9): 2026–2040.
25. Kirshtein B, Bayme M, Domchik S, Mizrahi S, Lantsberg L. Complicated appendicitis: laparoscopic or conventional surgery? World J Surg. 2007; 31(4): 744–749.
26. Lin HF, Lai HS, Lai IR. Laparoscopic treatment of perforated appendicitis. World J Gastroenterol. 2014; 20(39): 14338–14347.
27. Bombil I, Lunda WS, Maraj A. Laparoscopic appendicectomy for complicated appendicitis at Sebokeng Hospital. IOSR Journal of Dental and Medical Sciences 2015; 14(12): 65–69.
28. Talha A, El-Haddad H, Ghazal AE, Shehata G. Laparoscopic versus open appendectomy for perforated appendicitis in adults: randomized clinical trial. Surg Endosc. 2020; 34(2): 907–914.
29. Evasovich MR, Clark TC, Horattas MC, Holda S, Treen L. Does pneumoperitoneum during laparoscopy increase bacterial translocation? Surg Endosc 1996; 10(12): 1176–1179.
30. Gurtner GC, Robertson CS, Chung SC, Ling TK, Ip SM, Li AK. Efect of carbon dioxide pneumoperitoneum on bacteraemia and endotoxaemia in an animal model of peritonitis. Br J Surg 1995; 82(6): 844–848.
31. Gupta R, Sample C, Bamehriz F, Birch DW. Infectious complications following laparoscopic appendectomy. Can J Surg 2006; 49(6): 397–400.
32. Yau KK, Siu WT, Tang CN, Yang GP, Li MK. Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg 2007; 205(1): 60–65.
33. Yeom S, Kim MS, Park S, Son T, Jung YY, Lee SA, Chang YS, Kim DH, Han JK. Comparison of the outcomes of laparoscopic and open approaches in the treatment of periappendiceal abscess diagnosed by radiologic investigation. J Laparoendosc Adv Surg Tech A. 2014; 24(11): 762–769.
34. Taguchi Y, Komatsu S, Sakamoto E, Norimizu S, Shingu Y, Hasegawa H. Laparoscopic versus open surgery for complicated appendicitis in adults: a randomized controlled trial. Surg Endosc 2016; 30(5): 1705–1712.
35. St Peter SD, Adibe OO, Iqbal CW, Fike FB, Sharp SW, Juang D, Lanning D, Murphy JP, Andrews WS, Sharp RJ, Snyder CL, Holcomb GW, Ostlie DJ. Irrigation versus suction alone during laparoscopic appendectomy for perforated appendicitis: a prospective randomized trial. Ann Surg 2012; 256(4): 581–585.
36. Clark RA, Towbin R. Abscess drainage with CT and ultrasound guidance. Radiol Clin North Am. 1983; 21(3): 445–459.
37. Reynaert MS, Dardenne AN, Jacquemart JL, Kestens PJ. Percutaneous drainage of infected abdominal collections. Guiding principles and results. Acta Chir Belg. 1983; 83(5): 353–357.
38. Fernández M, Ortega D, Darrás A, Gallardo S, Yarmuch J. Percutaneous drainage of abdominal abscesses. Rev Med Chil. 1990; 118(7): 772–776.
39. Lin YM, Hsieh CH, Cheng CI, Tan BL, Liu HT. Laparoscopic appendectomy for complicated acute appendicitis does not result in increased surgical complications. Asian Journal of Surgery 2012; 35(3): 113–116.
40. Quezada F, Quezada N, Mejia R, Brañes A, Padilla O, Jarufe N, Pimentel F. Laparoscopic versus open approach in the management of appendicitis complicated exclusively with peritonitis: a single center experience. International Journal of Surgery 2015; 13: 80–83.
41. Mohamed AA, Mahran KM. Laparoscopic appendectomy in complicated appendicitis: Is it safe? J Minim Access Surg. 2013; 9(2): 55–58.
42. Dasari BVM, Baker J, Markar S, Gardiner K. Laparoscopic appendicectomy in obese is associated with improvements in clinical outcome: systematic review. Int J Surg. 2015; 13: 250–256.
43. Dumas RP, Subramanian M, Hodgman E, Arevalo M, Nguyen G, Li K, Aijwe T, Williams B, Eastman A, Luk S, Minshall C, Cripps MW. Laparoscopic Appendectomy: A Report on 1164 Operations at a Single-Institution, Safety-Net Hospital. Am Surg. 2018; 84(6): 1110–1116.
44. Athanasiou C, Lockwood S, Markides GA. Systematic Review and Meta-Analysis of Laparoscopic Versus Open Appendicectomy in Adults with Complicated Appendicitis: an Update of the Literature. World J Surg. 2017; 41(12): 3083–3099.
45. Quah GS, Eslick GD, Cox MR. Laparoscopic appendicectomy is superior to open surgery for complicated appendicitis. Surg Endosc. 2019; 33(7): 2072–2082.