Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2020, vol. 19(3–4), pp. 151–155 DOI: https://doi.org/10.15388/LietChirur.2020.19.35
eTep-retromuscular Repair for Ventral Hernia; a Technique Closest to Ideal
Aleksandar Mitevski
Department of Digestive Surgery, General Hospital RE-MEDIKA, Skopje, Macedonia
Goce Delchev University, Shtip, Macedonia
E-mail: aleksandar.mitevski@ugd.edu.mk (corresponding author)
Petar Markov
Goce Delchev University, Shtip, Macedonia
E-mail: petar.markov@ymail.com
Abstract. Introduction. Ventral hernia represents a problem for the surgeon and patients alike. eTEP repair is a technique that is minimally invasive, provides lower overall complication rates, decreased wound complications and the recurrence rates and shortens the length of stay in the hospital. Case. We present a case of a 48 year old patient who was admitted to our hospital for elective treatment of recurrent umbilical hernia. The patient had umbilical hernia repair 4 years ago, suture repair without mesh placement was performed according to the information given by the patient. On inspection there is visible supraumbillical scar, 12 cm in length with hernia bulging under the scar which is partially reducible on pressure. Discussion. The eTEP technique is closest to ideal because the abdominal cavity is not penetrated, is lessening the risk of visceral lesions and trocar site hernias, allows local or regional anesthesia, gives unsurpassed views of inguinal region and hernias and reproduces the technique of Rives-Stoppa. In favor to overcome the limitations deriving from the limited surgical field and restricted port set up, this technique has been modified based on the normal anatomy of the abdominal wall naming it dependently of the extension of the dissection and the location of the hernia. Conclusion. The extended-TEP (e-TEP) technique is based on the anatomical principle that the extraperitoneal space can be reached from almost anywhere in the anterior abdominal wall. It provides the most of the benefits for the patients but also requires great surgical skill and understanding of the anatomy of the anterior abdominal wall.
Key words: minimal invasive surgery, TEP, ventral hernia, laparoscopy, sublay.
Received: 2020/07/07. Accepted: 2020/08/21.
Copyright © 2020 Aleksandar Mitevski, Petar Markov. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Ventral hernia represents a problem for the surgeon and patients alike. Laparotomy has a burden present in incisional hernia rate around 20% and hernia recurrence rates also remain high especially considering the healthcare and societal costs [1, 2].
Technique selection process in every day practice includes patients who expect to have an active role in the process. Surgeons therefore have to narrow down the options based on potential benefits and deficiencies of the techniques and their application on different clinical scenario.
When searching for the ideal technique for ventral hernia, we need a technique that has low recurrence rate, has the least complications, it is minimal invasive, reduces postoperative recovery period, reduces and prevents a expenses and thus reduces the hospital stay.
eTEP (extended or enhanced view – Totaly Extra Peritoneal) repair is a technique that is minimally invasive, provides lower overall complication rates, decreased wound complications and the recurrence rates and shortens the length of stay in the hospital [3].
eTEP is a mesh hernia repair, using a mesh today is the most common in all techniques for ventral hernia and has decreased the longterm rate of recurrence from 63% for primary, non mesh repair to 32% [4]. eTEP technique uses prosthesis that is not expensive and easy to handle.
Case
We present a case of a 48 year old patient who was admitted to our hospital for elective treatment of recurrent umbilical hernia. The patient had umbilical hernia repair 4 years ago, suture repair without mesh placement was performed according to the information given by the patient. On inspection there is visible supraumbillical scar, 12 cm in length with hernia bulging under the scar which is partially reducible on pressure.
We used general anesthesia, in the left part of the epigastrium, over the left rectus abdominal muscle, a 12 mm incision is made through which the anterior vagina of abdominal rectus muscle is incised. The muscle fibers were bluntly divided and a 12 mm trocar was introduced in the retro-muscular space. We insufflated CO2 and a blunt dissection of the posterior sheath of rectus abdominis muscle was made from the rectus abdominis using 0 degree laproscope till 12 mm/Hg pressure was achieved and sufficient space is dissected. On the left semilunar line, 10 cm under the first one, 5 mm trocar was introduced. The medial part of the vagina of rectus abdominis muscle was opened, the falciform ligament is dissected and the vagina of the right rectus muscle is then opened. Complete retro-muscular dissection is conducted and two more trocars are introduced one at the right epigastrium and the other at the level of the umbilicus on the left semilunar line. The hernia sac was dissected to the point where it was intimately adhered to the thin layered skin (Figure 1). The hernia sac was transected and the omental adhesions were dissected from the sac. Retro-muscular space dissection was performed according to the principles of described by Rives-Stoppa (Figure 2). The hernia sac was closed with continuous 2–0/polydioxanon (PDS) barbed suture and the hernia defect with continuous 0/PDS barbed suture. 30×15 polipropylene mesh is placed in the retro-muscular space and a closed suction drainage was used for 1 day (Figure 3). Fixation of the mash was not used. The trocars were extracted under visualization and the space was gradually deflated under direct visualization. The incisions were closed with sutures.
Post operative recovery was uneventful, the drain was extracted on the first postoperative day and the patient was discharged from the hospital.
Abdominal hernia brace was applied for 1 month.
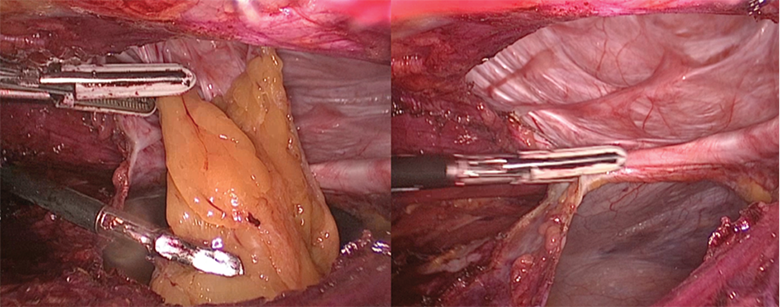
Figure 1. Adhesiolysis of greater omentum and transection of the hernial sac
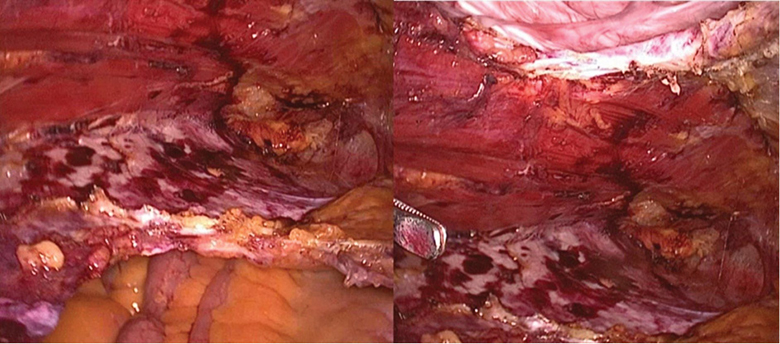
Figure 2. Creation of large retro-muscular space
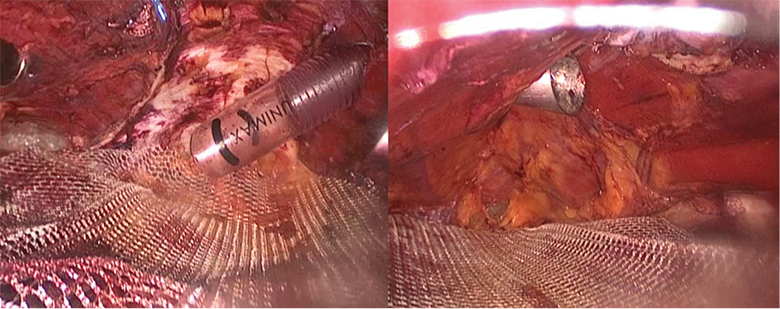
Figure 3. Placement of a large mesh without fixation
Discussion
When choosing a technique for hernia repair we strive to the ideal one. With TEP (totally extra peritoneal) technique peritoneal cavity is not entered which is lessening the risk of visceral lesions and trocar site hernias. It allows local or regional anesthesia, gives sufficient views of hernia not just in inguinal region but in other regions and reproduces the Rives-Stoppa principle. There are certain limitations to the TEP technique, which are limited surgical field and restricted port set up.
This technique has been modified in order to overcome the limitations described above. Changes were made based on the anatomy of the abdominal wall and the location of the hernia defect, thus respecting the extension of the dissection which enabled better view and more ergonomic port setup. In that respect it is named extended or enhanced view totally extraperitoneal technique (eTEP), eTEP Rives-Stoppa, eTEP TAR or eTEP Lumbar. Although it is referred as TEP, it’s not a real TEP technique because in most of the cases the surgeon must open the hernia sac, dissect the intra-abdominal adhesions and closes the hernia sac, thus going intra-peritoneal. Perhaps most correct name for the technique is an endoscopic retromuscular ventral hernia repair [5].
The retro-rectus repair, presented by Rives, later Stoppa and Wantz, revolutionized hernia repair by offering a robust treatment of complicated incisional hernias with a low recurrence rate [6, 7]. Contemporary series of the Rives-Stoppa technique reaffirmed the repair. When reports of a low hernia recurrence rate of 5%, an improved wound infection rate of 4% are combined with minimally invasive techniques, numbers are expected to go even lower [8].
eTEP is a technique which allows for a creation of a large surgical field with good visibility, flexible port set up, tolerance to pneumoperitoneum and better ergonomics.
This approach allows for a repair in more complex cases like selected ventral, incisional and lumbar hernias [9].
The principles that this method dictates are closure of the defect and restoration of the linea alba on the midline, usage of uncoated mesh and placing it outside the peritoneal cavity, minimal or none fixation of mesh without compromising the hernia repair and offers sustainable minimal invasive approach.
It is very important that the port placement is in the correct anatomical plane (retro-rectus space), respecting the angulations’ principle and allowing the best approach to the defect.
Placement of the mesh in a created sublay space minimizes mesh migration or folding, thus allowing for less penetrating fixation and thereafter less chronic pain. Also, the wound complications from 27–30% in open approach have been dramatically dropped down.
The placement of the mesh in the retro-muscular space (sublay) spares the perforating vessels and avoids skin and musculofascial flaps, decreasing the risk for ischemia and wound complications [10].
On other hand the technique is very technically challenging and the surgeon have to understand the relationship between spaces [11].
As the prosthesis is placed in sublay fashion – extraperitoneally, uncoted mesh is used so it has a lower price and reduced the risk of adhesions [12].
Conclusion
There are many available minimally invasive techniques for repair of ventral hernia. Surgeons should be proficient in most if not in all of them in order to accommodate to patient’s needs and to be able to convert from one to another when necessary.
The extended view TEP (eTEP) technique is based on the anatomical principle that the extraperitoneal space can be reached from almost anywhere in the anterior abdominal wall. It provides the most of the benefits for the patients but also requires great surgical skill and understanding of the anatomy of the anterior abdominal wall.
References
1. Burger JWA, Halm JA, Wisjmuller AR, ten Raa S, Jeekel J. Evaluation of new prosthetic meshes for ventral hernia repair. Surg Endosc 2006; 20(8): 1320–1325.
2. Cassar K, Munro A. Surgical treatment of incisional hernia. Br J Surg 2002; 89(5): 534–545.
3. Pierce RA, Spitler JA, Frisella MM, Matthews BD, Brunt LM. Pooled data analysis of laparoscopic vs. open ventral hernia repair: 14 years of patient data accrual. Surg Endosc 2007; 21(3): 378–386.
4. Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 2004; 240(4): 578–583.
5. Daes J. The extended-view totallyextraperitoneal (eTEP) technique for inguinal hernia repair. In: Novitsky YW, ed. Hernia Surgery. Cham: Springer, 2016, 467–472.
6. Rives J, Lardennois B, Pire JC, Hibon J. Large incisional hernias. The importance of flail abdomen and of subsequent respiratory disorders. Chirurgie 1973; 99(8): 547–563.
7. Stoppa RE. The treatment of complicated groin and incisional hernias. World J Surg 1989; 13(5): 545–554.
8. Iqbal CW, Pham TH, Joseph A, Mai J, Thompson GB, Sarr MG. Long-term outcome of 254 complex incisional hernia repairs using the modified Rives-Stoppa technique. World J Surg 2007; 31(12): 2398–2404.
9. Daes J. The enhanced view – totally extraperitoneal technique for repair of inguinal hernia. Surg Endosc 2012; 26(4): 1187–1189.
10. Novitsky Y, Porter J, Rucho ZC, Getz S, Pratt B, Kercher K, Heniford B. Open preperitoneal retrofascial mesh repair for multiply recurrent ventral incisional hernias. Journal of American College of Surgeons 2006; 203(3): 283–289. DOI: 10.1016/j.jamcollsurg.2006.05.297.
11. Belyansky I, Daes J, Radu VG, Balasubramanian R, Reza Zahiri H, Weltz AS, Sibia US, Park A, Novitsky Y. A novel approach using the enhanced – view totally extraperitoneal (eTEP) technique for laparoscopic retromuscular hernia repair. Surg Endosc 2018; 32(3): 1525–1532. DOI: 10.1007/s00464-017-5840-2.
12. Radu VG, Lica M. The endoscopic retromuscular repair of ventral hernia: the eTEP technique and early results. Hernia 2019; 23(5): 945–955. DOI: 10.1007/s10029-019-01931-x.