Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2021, vol. 20(1), pp. 27–31 DOI: https://doi.org/10.15388/LietChirur.2021.20.38
Low-grade Appendiceal Mucinous Neoplasm (Appendiceal Villous Adenoma) with Cystic Fibrosis: A Case Report
Emrah Doğan
Department of Radiology, Faculty of Medicine, Muğla Sıtkı Koçman University, Turkey
E-mail: dr_e_dogan@hotmail.com
Hakan Avcı
Department of General Surgery, Ayvalik State Hospital, Turkey
E-mail: hhakanavci@hotmail.com
Muge Kuzu Avcı
Department of Pediatrics, Ayvalik State Hospital, Turkey
E-mail: mugekuzu@hotmail.com
Korkut Bozkurt
Department of Pathology, Muğla Milas State Hospital, Turkey
E-mail: kbozkurt78@gmail.com
Ozge Oral Tapan
Department of Pulmonology, Faculty of Medicine, Muğla Sıtkı Koçman University, Turkey
E-mail: dr.utkutapan@yahoo.com
Utku Tapan
Department of Pulmonology, Faculty of Medicine, Muğla Sıtkı Koçman University, Turkey
E-mail: ozgeeoral@hotmail.com
Abstract. Cystic fibrosis (CF) is an autosomal dominant disease characterized by the dysfunction of exocrine secretory glands resulting from a mutation in the transmembrane regulator protein (CFTR) gene. As life expectancy increases in patients with cystic fibrosis secondary to advances in treatment, advanced age malignancies secondary to cystic fibrosis emerge. Especially, the frequency of gastrointestinal system malignancies and colon cancers increases with aging. Appendiceal tumors are a rare entity and constitute less than 1% of gastrointestinal tumors. We presented a villous adenoma encountered in an 18-year-old male patient with CF accompanied by clinical and radiological findings. Our case is the first reported appendiceal tumor that emerged in patients with cystic fibrosis.
Key words: appendiceal tumors, cystic fibrosis, appendectomy.
Received: 2020/11/05. Accepted: 2021/02/03.
Copyright © 2021 Emrah Doğan, Hakan Avcı, Muge Kuzu Avcı, Korkut Bozkurt, Ozge Oral Tapan, Utku Tapan. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Cystic fibrosis (CF) is an autosomal dominant disease characterized by the dysfunction of exocrine secretory glands resulting from a mutation in the transmembrane regulator protein (CFTR) gene [1]. Disruption of chlorine transport changes mucus viscosity. As a result, the barrier effect is lost in the organs protected by mucus, and the exposure to carcinogens and irritants increases. Consequently, the development of malignancy is increasing [2].
As life expectancy increases in patients with cystic fibrosis, older age tumors affecting the patients appear. According to the literature, the frequency of gastrointestinal malignancies and colon cancers increases in the 3rd and 4th decades [3]. We presented an appendiceal tumor encountered in an 18-year-old male patient with CF accompanied by clinical and radiological findings. Our case is the first reported appendiceal villous adenoma that emerged in patients with cystic fibrosis.
Case report
An 18-year-old male patient was admitted to our hospital with abdominal pain. In the anamnesis and history, it was reported that the patient was first hospitalized at the age of 40 days with a cough complaint. He was suffering from frequent upper respiratory tract infections. Unfortunately, CF was not noticed until 2014. Our patient’s problem was supposed as asthma. He was given inhaler treatment in hospital admissions. The hand X-ray in 2014 showed that the patient followed the developmental stages 1.5 years behind. Our patient was diagnosed with CF in 2014 when admitted to the hospital with several problems such as green-colored mucus with cough, steatorrhea, and excessive sweating.

Figure 1. Bilaterally interstitial reticular densities and tram-tract appearance due to bronchiectasis in X-ray graph
In the systemic examination, bilaterally rales were present in lung auscultation. The peripheral pulses were normal. S1 and S2 were rhythmic, with no murmur, in normal sinus rhythm. In the laboratory, the neurological examination was normal. In X-ray chest graph, bilaterally tram-track linear opacities were observed [Figure 1]. These signs were interpreted as bronchiectasis due to CF. The patient had defences and rebound in the abdominal examination. WBC was 14,000×109/L. In the USG, the appendix was distended and no taken response to compression. He was operated on with a preliminary diagnosis of acute appendicitis. Unfortunately, since this rare diagnosis of the patient was not predicted, no images were obtained during the operation and sonographically.
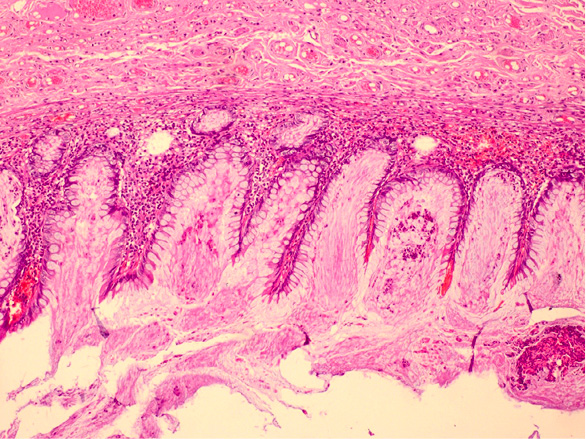
Figure 2. Villiform mucinous epithelial proliferation appears to replace the normal appendix mucosa
Pathologically, the appendix lumen diameter was 1.7 cm in the widest area. The appendix’s long axis was 7.5 cm. Mucoid material was observed in the lumen. The pathologic diagnosis was low-grade appendiceal mucinous neoplasm (appendiceal villous adenoma). Villiform mucinous epithelial proliferation was observed to replace the normal appendix mucosa [Figure 2]. It was observed that lymphoid tissue decreased In lamina propria and was replaced with fibrotic connective tissue [Figure 3]. Villiform mucinous epithelial proliferation appears to be composed of long mucinous epithelial cells with a low degree of nuclear atypia [Figure 4].
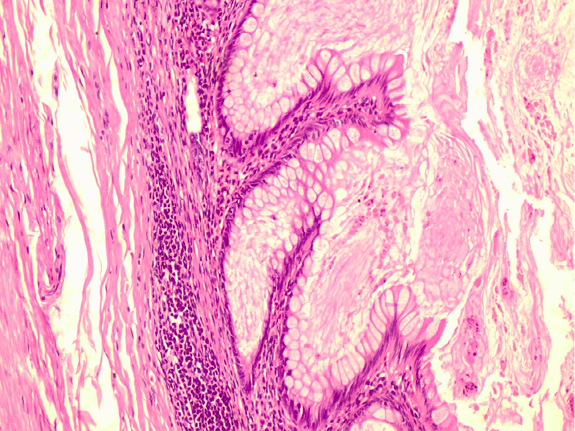
Figure 3. In the lamina propria, it is observed that lymphoid tissue decreases, instead, fibrotic connective tissue passes
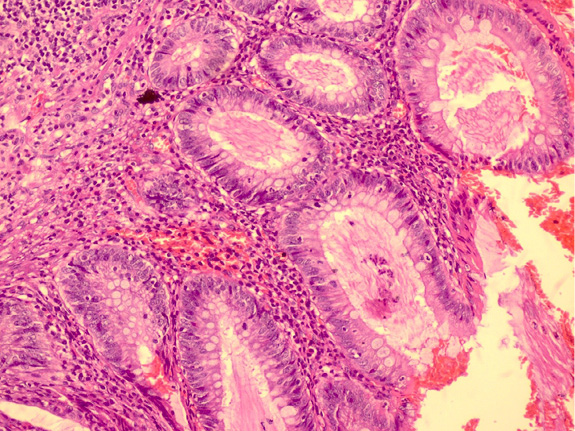
Figure 4. Villiform mucinous epithelial proliferation consisting of long mucinous epithelial cells with low degree of nuclear atypia
Discussion
Appendix lesions are seen rarely. The incidence of appendiceal tumors is less than 0.4% of gastrointestinal neoplasms [4]. This case is the first reported appendix villous adenoma in the literature. Appendix tumors are rarely symptomatic at the beginning. Then, an obstruction and accompanying infection is concluded appendicitis [5]. Thereby, probable clinic presentation is appendicitis. However, many routine reasons are leading to lower quadrant pain in the patient with CF. Distal ileal obstruction syndrome (DIOS) is generally the responsible reason [6]. The other causes of lower abdominal pain are intussusception, volvulus, pancreatitis, and fecalith. Clinic table resulting from the pathologies mentioned above can mimic appendicitis. Therefore, the differential diagnosis of appendicitis in patients with cystic fibrosis is different from normal patients. Furthermore, the radiological assessment is not useful too. The appendix size exceeds 6 mm (upper limit of the normal appendix) due to mucus distension. As it is well known, the size of the appendix, erected appearance, and distension the most useful diagnostic radiological criteria in appendicitis. The normal appendix in CF is fulfilled all of this criterion. However, knowing the difference of evaluation in CF prevents misdiagnosis. However, an appendix lesion like a small villous adenoma can only be detected incidentally [7, 8].
Once you detected an adenoma in GIS, further evaluation is necessary. Accompanying adenomas may be observed in any area of the intestinal tract. The most remarkable feature of this type of lesion is atypia. Atypia is frequent in CF because of the factors such as disruption of the protective barrier, changes in the fecal microbiome, and dysmotility. Adenomas are a stepping stone of the cancer process in the colon and other intestinal as well as the appendix cancers. The villous adenomas of the appendix occupy a large area of the appendix mucosa. The mucosa is the shape of papillary leaves surrounded by a large number of cells that produce mucus. It looks deceptively harmless. The dysplasia can be evaluated by detecting atypia in the basal cells. Serrated patterns may be seen in suspected areas. Epithelial cells can mimic the mucocele of the appendix [9–11].
Conclusion
The diagnosis of appendicitis is problematic clinically and radiologically in patients with CF owing to distention of the appendix resulting from mucus retention. The appendix tumor is rarely seen in CF. We observed an appendix tumor incidentally. Our case is the first villous adenoma in a patient with CF. The clinical significance of the lesion is being a stepping stone for malignancies revealing at advanced ages. Today, life expectancy has exceeded the age of 45 in CF and will continue to increase. Malignancies will occupy more place among mortality reasons, instead of respiratory failure, chronic progressive pulmonary disease, acute pancreatitis, heart, lung, or kidney failures. Considering all of these, the significance of atypia revealed in the early age group will be increased [5]. This subject still needs new cases.
References
1. Goetz D, Ren CL. Review of Cystic Fibrosis. Pediatr Ann 2019; 48(4): e154–e161. DOI: 10.3928/19382359-20190327-01.
2. Sommerburg O, Schenk JP. Abdominelle Manifestationen bei Mukoviszidose: Klinische Übersicht [Abdominal manifestations in cystic fibrosis: Clinical review]. Radiologe 2020; 60(9): 781–790. DOI: 10.1007/s00117-020-00729-8.
3. Hough NE, Chapman SJ, Flight WG. Gastrointestinal malignancy in cystic fibrosis. Paediatr Respir Rev 2020; 35: 90–92. DOI: 10.1016/j.prrv.2020.03.002.
4. Ruoff C, Hanna L, Zhi W, Shahzad G, Gotlieb V, Saif MW. Cancers of the appendix: review of the literatures. ISRN Oncol 2011; 2011: 728579. DOI: 10.5402/2011/728579.
5. Evola G, Caruso G, Caramma S, Dapri G, Spampinato C, Reina C, Reina GA. Tubulo-villous adenoma of the appendix: A case report and review of the literature. Int J Surg Case Rep 2019; 61: 60–63. DOI: 10.1016/j.ijscr.2019.06.061.
6. Green J, Gilchrist FJ, Carroll W. Interventions for preventing distal intestinal obstruction syndrome (DIOS) in cystic fibrosis. Cochrane Database Syst Rev 2018; 6(6): CD012619. DOI: 10.1002/14651858.CD012619.pub2.
7. Sabharwal S. Gastrointestinal Manifestations of Cystic Fibrosis. Gastroenterol Hepatol (N Y) 2016; 12(1): 43–47.
8. Rud B, Vejborg TS, Rappeport ED, Reitsma JB, Wille-Jørgensen P. Computed tomography for diagnosis of acute appendicitis in adults. Cochrane Database Syst Rev 2019; 2019(11): CD009977. DOI: 10.1002/14651858.CD009977.pub2.
9. Yamada A, Komaki Y, Komaki F, Micic D, Zullow S, Sakuraba A. Risk of gastrointestinal cancers in patients with cystic fibrosis: a systematic review and meta-analysis. Lancet Oncol 2018; 19(6): 758–767. DOI: 10.1016/S1470-2045(18)30188-8.
10. Abraham JM, Taylor CJ. Cystic Fibrosis & disorders of the large intestine: DIOS, constipation, and colorectal cancer. J Cyst Fibros 2017; 16: S40–S49. DOI: 10.1016/j.jcf.2017.06.013.
11. Karmarkar P, Joshi A, Wilkinson A, Mahore S, Bothale K. Villous adenoma of the appendix with dysplasia. Saudi J Gastroenterol 2008; 14(1): 38–39. DOI: 10.4103/1319-3767.37807.