Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2022, vol. 21(3–4), pp. 229–235 DOI: https://doi.org/10.15388/LietChirur.2022.21.70
Surgical Treatment of Finger Degloving Injuries Without Usable Skin: a Case Report and Literature Review
Agnius Stulpinas
Faculty of Medicine, Vilnius University, Vilnius, Lithuania
E-mail: ag.stulpinas@gmail.com
Rūta Venciūtė-Stankevičė
Center of Plastic and Reconstructive Surgery, Vilnius University Hospital Santaros Klinikos, Vilnius, Lithuania
E-mail: venciute.ruta@gmail.com
Nerijus Jakutis
Faculty of Medicine, Vilnius University, Vilnius, Lithuania
Center of Plastic and Reconstructive Surgery, Vilnius University Hospital Santaros Klinikos, Vilnius, Lithuania
E-mail: Nerijus.jakutis@santa.lt
Abstract. The treatment of avulsion injuries of the fingers is complicated by the lack of universally accepted treatment guidelines and the wide variety of reconstruction techniques. The aim of this paper is to present a case and review the scientific literature to provide clear criteria for amputation and reconstruction and to present and discuss the reconstruction techniques with the best results.
Key words: free flaps, finger avulsion, finger reconstruction, finger degloving.
Received: 2022/05/12. Accepted: 2022/07/28.
Copyright © 2022 Agnius Stulpinas, Rūta Venciūtė-Stankevičė, Nerijus Jakutis. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Degloving soft tissue injuries (DSTI) are a type of avulsion injuries that consists of separation of a portion of the skin and subcutaneous tissue from the subcutaneous fascia, tendon sheaths, bones and muscles. These injuries can affect any part of the body, but the lower limbs, face and neck, back and upper limbs are the most commonly affected [1]. DSTI often involves concomitant damage to deeper anatomical structures, most commonly nerves, blood vessels, bones and tendons [2]. The main principles of treatment of DSTI are rapid diagnosis, excision of non-viable tissue, skeletal fixation if fractures are present, and replantation of the amputated body part. After replantation, a series of reconstructive surgeries follow, with the aim of restoring the lost function of the amputated limb [3, 4]. The basic functions of the hand and fingers are severely affected by DSTI: the manipulator function of the hand, the grasping function of the fingers, the opposing function of the thumb, and the tactile sensation of the fingers, it is therefore essential to restore these functions by replantation or reconstruction of the affected part. However, due to the individual nature of each injury, this is not always possible. The choice of surgical treatment is also complicated by the lack of universally accepted treatment guidelines and the fact that the scientific literature is dominated by general treatment principles and case reports. The aim of this case report is to review the choice of replantation or amputation, the latest and most successful surgical treatment methods for DSTI of the fingers, and to explain the treatment in Vilnius University Hospital Santaros Clinics.
Case report
A 56-year-old woman had her hand caught between rollers at 9.30 on 08/03/2022 while at work. The patient was taken by an ambulance to the Emergency Department of Vilnius University Hospital Santaros Clinics, examined by an orthopedic traumatologist and a plastic-reconstructive surgeon (Fig. 1). The examination revealed an avulsion amputation of the skin of the II finger up to the middle third of the proximal phalanx, damage to the neurovascular bundle of the II finger, the metacarpal bones, flexor and extensor tendons were spared. Amputations of the distal phalanges of fingers IV and V. Diagonal fracture of the body of the middle phalanx of finger IV without significant dislocation. Amputated skin was not recovered. Diagnosis: crushing injury to the right hand. Avulsion amputation of fingers II and IV, amputation of the distal phalanx of finger V, avulsion fracture of the middle metacarpal of finger IV, III finger wound. The patient was referred to an orthopedic traumatologist for amputation of fingers II, V and stump formation, stump formation of finger IV. The patient was hospitalized urgently for surgical treatment. Blood tests results were without significant abnormalities. Surgery performed on 08/03/2022 at 19.30: wounds revised, massive debridement with removal of non-viable soft tissues and bone fragments. Amputations of the II and the V finger at the proximal phalanx level. IV finger stump was formed over the distal phalanx. On 10/03/2022 the patient was discharged for outpatient treatment after clarification of recommendations. Results after 6 weeks (Fig. 2).

Figure 1. Preoperative state
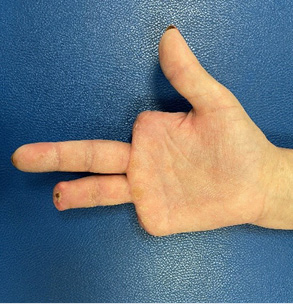


Figure 2. It should be noted that the distal thirds of the II and V metacarpals were not removed during the operation, but the patient is satisfied with the functional state – it is comfortable to grip a pen
Discussion
DSTI of the fingers is a particularly difficult problem to treat because of the extent of damage to the skin and subcutaneous tissue, nerves and blood vessels. The first step after identifying DSTI of the fingers is the selection of patients for replantation, as successful replantation does not always result in satisfactory preservation of finger function. For example, a non-mobile thumb replanted in an opposable position is valuable for pinching and grasping, whereas other inflexible fingers may lead to deterioration in hand function [5]. Several classification systems have been developed for more efficient treatment selection [6–8] and these systems allow patients to be categorized according to the intended treatment and functional outcome (Table 1).
Table 1.
|
Urbaniak classification |
||
|
Class |
Description |
Treatment |
|
I |
Avulsion injury with sufficient blood supply. |
Soft tissue and bone treatment |
|
II |
Incomplete avulsion injury with inadequate blood supply. |
Revascularization |
|
III |
Avulsion injury with complete degloving or amputation. |
Amputation |
|
Kay classification modified by Adani |
||
|
I |
Avulsion injury with sufficient blood supply. |
Soft tissue and bone treatment |
|
II IIa IIv |
Incomplete avulsion injury with inadequate venous/arterial circulation, without skeletal injury. Insufficient arterial circulation only. Insufficient venous circulation only. |
Revascularization |
|
III IIIa IIIv |
Incomplete avulsion injury with inadequate venous/arterial circulation, with skeletal or joint injury. Insufficient arterial circulation only. Insufficient venous circulation only. |
Amputation/reconstruction |
|
IV IVp IVd |
Avulsion injury with complete degloving or amputation. Proximal to the flexor digitorum superficialis tendon insertion. Distal to the flexor digitorum superficialis tendon insertion. |
Only degloving – amputation/reconstruction Amputation Amputation/reconstruction |
The modified Kay classification is important because it divides Urbaniak class II into 2 classes: without skeletal injury and with skeletal injury. According to the authors’ data, when comparing II Kay with III Kay, the operative treatment of II Kay injuries was more successful in terms of revascularization (73% and 86%, respectively) and amplitude of active motion above 90° (57% and 100% of patients respectively). Similarly, the treatment of Kay class III injuries required arthrodesis of the distal interphalangeal joint in 50% of cases, and more than one operative procedure was performed in 83.3% of cases (compared with 36.4% in Kay II): split-skin grafting, revision of venous insufficiency, treatment of infection of the proximal interphalangeal joint, late arthrodesis of the distal interphalangeal joint, and secondary amputation [7]. Adani’s publication extends Kay’s class IV according to anatopathology: amputations proximal to the flexor digitorum superficialis insertion have a poorer postoperative prognosis and finger amputation is recommended, while those distal to the insertion have a more favorable prognosis, and degloving injuries with intact tendons and bones is likely to have a successful cutaneous revascularization and an optimal aesthetic and functional outcome [8].
Careful selection of patients and expected functional outcomes help to answer important pre-operative questions: will grasping improve? Will the finger be flexible? Will satisfactory finger sensitivity remain? For how long will the patient be unable to work? Will the patient be able to continue working? Will the aesthetic appearance be satisfactory? Is the patient healthy enough for a longer operation? What is the likelihood of healing? How many more operations will be required?
When making treatment decisions, it must be remembered that the final functional outcome is not only determined by the injury, but also by the patient’s age, health, general expectations, adherence to rehabilitation, psychosocial attitudes and other factors (Table 2) [5]. The operative treatment of each injury must be individualized, taking into account the complexity, the extent of the injury and the combination of these variables. The surgeon must emphasize that the patient must be committed to a regimen that requires rigorous rehabilitation. It is likely that the finger will become functional only 12–18 months after the injury [9]. If the patient is unable to commit to this, replantation or reconstruction becomes contraindicated.
Table 2.
|
Prognostic indicators for poor outcome after replantation |
|
Crushing/avulsion injury |
|
“Red Line” sign The red line sign, which refers to an avulsion injury, is clinically visible as a red band of ecchymosis along the lateral edge of the finger. This ecchymosis is caused by bleeding from the branches of the finger artery that have been severed after traumatic injury [10]. |
|
“Ribbon” sign The ribbon sign, which also refers to an avulsion injury, is a kink in the digital artery resulting from damage to the layers of the blood vessel wall. When these signs (red line and/or band) are present, the area of injury must be bypassed with vein grafts when attempting to replant [10]. |
|
Warm ischemia > 6 hours |
|
Cold ischemia > 12 hours |
|
Multilevel injury |
|
Extensive bone loss |
|
Nerve loss |
|
Multiple joint disruption |
|
Advanced age |
|
Poor candidate for immobilization |
|
Psychosocial disturbance |
|
Rehabilitation compliance concerns |
In the case described in this paper, amputation of the II finger was chosen for several reasons: the neurovascular bundle was torn, the severed skin was not brought to the hospital and the treatment was discussed with the patient – reconstruction is only possible with flaps from other parts of the body, the choice of this treatment would lead to a prolonged disability and lengthy sick leave, and so the patient opted for amputation.
Revascularization or replantation, when possible, is the ideal treatment for avulsion trauma [11, 12]. However, reconstruction of the finger in the absence of avulsed tissues can be performed using free flaps. The choice of the flap depends on the surgeon’s experience and the extent of the injury. In the case of one or two fingers, the flap used for reconstruction should be thin, flexible, wide enough to encircle the affected fingers and easily prepared. It is therefore advantageous to use free fasciocutaneous flaps, as they take thin, vascularized tissue, together with fascia, which is used for tendon sliding.
Innervated arterialized venous flap from the dorsal surface of the foot [13]: this flap has the highest sensitivity of the flaps reviewed, averaging 6 mm in 2-point discrimination (2PD) tests. The donor flap is made of thin and flexible skin, resulting in a better aesthetic outcome. It is worth mentioning that the transfer of this flap can be performed by 2 teams, resulting in shorter operating times. The donor site is aesthetically well localized, as it is not visible when wearing shoes. The main problem with flaps from the dorsal foot region is the long healing time of the donor site, which may be complicated by purulent infection or osteomyelitis [14, 15]. The relative disadvantages of this flap are that in men the donor site is often hairy, hence poorer and the donor site may be painful when wearing shoes.
Free radial forearm flap [16]: it is used as a sensitive patch for medium to large defects. This flap has a reliable perforating artery and the flap matches the skin color of the fingers and allows for a 2-team operation. A local sensory nerve can be harvested with the flap if necessary, but the 2-point discrimination test did not show a significant difference between the sensitive and non-sensitive groups during the follow-up period (8–13 mm). Protective sensation recovered within one year in patients with insensitive patches. This suggests that nerve harvesting is not compulsory, thus, shorter operating time. The disadvantages of this flap are the removal of a major local artery and an unsightly scar in the donor area.
Spiraled parallelogram medial arm free flap [17]: the inner surface of the upper arm is the donor site for a thin, hairless patch of skin with a well-hidden scar and, if necessary, a sensory nerve can be harvested simultaneously. These flaps have good functional and cosmetic results due to the thin, flexible skin of the flap donor sites, with an average score of 8–9 mm in 2PD tests. It should be noted that due to the anatomical variation of the vasculature, more careful preoperative preparation is required. The authors also note that poor venous outflow is a potential disadvantage of this approach, but this disadvantage can be overcome by taking a larger flap than with traditional flap design criteria. In addition, all patients in the study were thin, so this flap is not recommended for patients with thick subcutaneous tissue.
The total active movement range (TAM) of the fingers reconstructed with these flaps did not differ significantly, all had good or excellent results according to the ASSH scale [18] (Good: >75%, Excellent: same flexibility as the other hand on the same finger), the cosmetic results were satisfactory, and the overall satisfaction of the patients with the final result was also high, suggesting that the surgeon’s experience with a particular flap grafting technique is the most important factor in the choice of the surgical approach. The methods described below are only suitable in cases where the neurovascular bundle was left intact during the injury.
Double cross-finger flap [19]: this method is characterized by the fact that it does not require a free flap from other anatomical regions. The authors reported good functional results, with a TAM of 120–145° and satisfactory sensitivity, with a 2PD of 9–11 mm, which is good considering that these flaps do not involve nerve suturing, although most patients complained of cold intolerance in the donor and recipient fingers. However, the use of this method is limited: it is not applicable to patients over 40 years of age, with Dupuytren’s syndrome, rheumatoid arthritis, etc. as the immobilization of the fingers (21 days on average) puts them at high risk of joint contractures. In addition, this flap transfers the hair of the adjacent finger onto the palmar surface of the injured finger and places the donor surface on the dorsum of the hand, and is therefore not recommended for women for aesthetic reasons. Compared to free flap techniques, this method is simpler as it does not require a microsurgical technique, but this means that it can only be used in cases where the neurovascular bundle is intact. Also, this flap is only suitable for isolated DSTI of the III or IV fingers, as it requires 2 healthy adjacent fingers, but this problem can be solved with the Open Book flap [20]: it is a similar procedure, with similar indications, but using one healthy adjacent finger as the donor area.
Using skin matrices [21]: the major advantages of this method are that it does not require a donor area for skin flap, a split skin graft is sufficient, thus avoiding donor area morbidity, and it is possible to operate on elderly patients or those with severe comorbidities, as local anesthesia is sufficient. Functional and aesthetic results are also good, fingers reconstructed using this technique are not thick and the TAM was excellent or good on the ASSH scale in more than half of the patients. The 2PD test results were excellent (6 mm) and good (7–15 mm) in 11% and 83% of patients respectively. According to the authors, patient satisfaction with the results was high due to good functional results and rapid healing, with patients’ fingers healing after a mean of 40 days. However, this method is not applicable when the neurovascular bundle is damaged and another problem is the high cost of the surgery – the use of skin matrices is expensive, but the cost problem is compensated by the short hospital stay, as patients were discharged on an outpatient basis on the day after the surgery, with weekly hospital follow-ups.
Finger reconstruction can be performed using pedunculated flaps from the groin, trunk or the opposite hand [22–27]. However, the disadvantage of these techniques is that the hand has to be fixed to the donor area for at least 2 weeks, which usually leads to joint stiffness due to prolonged immobilization. Another disadvantage of these techniques is that these patches are thick, requiring multiple thinning procedures in several steps. Joint movements often remains limited, sensory recovery and the appearance of the reconstructed fingers are rarely satisfactory [28]. However, if the skin of three or more fingers is avulsed, these flaps become the only reconstructive option, as all fingers can be covered at once with a single operation.
Conclusions
Patient selection is crucial in cases of DSTI of the fingers, and should focus on the psychosocial state of patients and their disposition to long-term post-operative treatment. If the injury involves one or two fingers, we recommend the surgical techniques described in this article, which have good functional and aesthetic results. There are many methods of finger reconstruction presented in the scientific literature, so it is important to remember that the best results will be achieved with the method chosen and refined by the surgeon.
Funding. This research received no external funding.
Informed consent statement. Written informed consent was obtained from the patient for anonymized patient information to be published.
Conflict of interest statement. The authors declare no conflict of interest.
References
1. Hakim S, Ahmed K, El-Menyar A, Jabbour G, Peralta R, Nabir S, Mekkodathil A, Abdelrahman H, Al-Hassani A, Al-Thani H. Patterns and management of degloving injuries: a single national level 1 trauma center experience. World Journal of Emergency Surgery 2016; 11(1): 35.
2. Velazquez C, Whitaker L, Pestana IA. Degloving Soft Tissue Injuries of the Extremity: Characterization, Categorization, Outcomes, and Management. Plast Reconstr Surg Glob Open 2020; 8(11): e3277.
3. Arnez ZM, Khan U, Tyler MPH. Classification of soft-tissue degloving in limb trauma. J Plast Reconstr Aesthet Surg 2010; 63(11): 1865–1869.
4. Eccles S (ed.). Standards for the management of open fractures. First edition. Oxford, New York, NY: Oxford University Press, 2020.
5. Medling BD, Bueno RA, Russell RC, Neumeister MW. Replantation outcomes. Clin Plast Surg 2007; 34(2): 177–185, VII–VIII.
6. Urbaniak JR, Evans JP, Bright DS. Microvascular management of ring avulsion injuries. The Journal of Hand Surgery 1981; 6(1): 25–30.
7. Kay S, Werntz J, Wolff TW. Ring avulsion injuries: Classification and prognosis. The Journal of Hand Surgery 1989; 14(2, Part 1): 204–213.
8. Adani R, Castagnetti C, Busa R, Caroli A. Ring avulsion injuries: microsurgical management. J Reconstr Microsurg 1996; 12(3): 189–194.
9. Chiu DTW, Matthew MK, Patel A. The Impact of Microsurgery on the Treatment of Ring Avulsion Injuries. Plastic and Reconstructive Surgery 2019; 144(6): 1351–1357.
10. Van Beek AL, Utz JEK, Zook EG, de Castro CC. Importance of the Ribbon Sign, Indicating Unsuitability of the Vessel, in Replanting a Finger. Plastic and Reconstructive Surgery 1978; 61(1): 32–39.
11. Krishnamoorthy R, Karthikeyan G. Degloving injuries of the hand. Indian J Plast Surg 2011; 44(2): 227–236.
12. Sears ED, Chung KC. Replantation of Finger Avulsion Injuries: A Systematic Review of Survival and Functional Outcomes. J Hand Surg Am 2011; 36(4): 686–694.
13. Takeuchi M, Sakurai H, Sasaki K, Nozaki M. Treatment of finger avulsion injuries with innervated arterialized venous flaps. Plast Reconstr Surg 2000; 106(4): 881–885.
14. Russo A, Delia G, Casoli V, Colonna MR, Stagno d’Alcontres F. Dorsalis Pedis Adipofascial Perforator flap for great toe reconstruction: anatomical study and clinical applications. J Plast Reconstr Aesthet Surg 2014; 67(4): 550–554.
15. Samson MC, Morris SF, Tweed AEJ. Dorsalis Pedis Flap Donor Site: Acceptable or Not? Plastic & Reconstructive Surgery 1998; 102(5): 1549–1554.
16. Lin C, Chen S, Chen T, Dai N, Chang S. Free fasciocutaneous flaps for reconstruction of complete circumferential degloving injury of digits. Microsurgery 2013; 33(3): 191–197.
17. Chi Z, Gao W, Yan H, Li Z, Chen X, Zhang F. Reconstruction of Totally Degloved Fingers With a Spiraled Parallelogram Medial Arm Free Flap. The Journal of Hand Surgery 2012; 37(5): 1042–1050.
18. Libberecht K, Lafaire C, Van Hee R. Evaluation and Functional Assessment of Flexor Tendon Repair in the Hand. Acta Chirurgica Belgica 2006; 106(5): 560–565.
19. Abo-hashem Azab Moosa A. Double Cross-Finger Flaps: A Novel Technique for Management of Ring Avulsion Injuries. Annals of Plastic Surgery 2010; 64(4): 409–411.
20. Tadiparthi S, Akali A, Felberg L. The “Open Book” Flap: A Heterodigital Cross-Finger Skin Flap and Adipofascial Flap for Coverage of a Circumferential Soft Tissue Defect of a Digit. J Hand Surg Eur Vol 2009; 34(1): 128–130.
21. Maruccia M, Marannino PC, Elia R, Ribatti D, Tamma R, Nacchiero E, Manrique OJ, Giudice G. Treatment of finger degloving injury with acellular dermal matrices: Functional and aesthetic results. Journal of Plastic, Reconstructive & Aesthetic Surgery 2019; 72(9): 1509–1517.
22. Chuang DC, Colony LH, Chen HC, Wei FC. Groin flap design and versatility. Plast Reconstr Surg 1989; 84(1): 100–107.
23. Yamada N, Ui K, Uchinuma E. The use of a thin abdominal flap in degloving finger injuries. British Journal of Plastic Surgery 2001; 54(5): 434–438.
24. Nazerani S, Motamedi MHK, Nazerani T, Bidarmaghz B. Treatment of Traumatic Degloving Injuries of the Fingers and Hand: Introducing the “Compartmented Abdominal Flap”. Techniques in Hand & Upper Extremity Surgery 2011; 15(3): 151–155.
25. Buja Z, Arifi H, Hoxha E. Repair of degloving fingers with abdominal tunnelization flap. J Hand Surg Eur Vol 2013; 38(4): 439–440.
26. McGeorge DD, Stilwell JH. The Management of the Complete Ring Avulsion Injury. Journal of Hand Surgery 1991; 16(4): 413–414.
27. Ng SW, Teoh LC, Lee YLJ, Seah WTV. Contralateral Pedicled Lateral Arm Flap for Hand Reconstruction. Annals of Plastic Surgery 2010; 64(2): 159–163.
28. Chen SL, Chou GH, Chen TM, Wang HJ. Salvage of completely degloved finger with a posterior interosseous free flap. Br J Plast Surg 2001; 54(1): 69–71.