Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2022, vol. 21(3–4), pp. 243–247 DOI: https://doi.org/10.15388/LietChirur.2022.21.72
Extranodal Diffuse Large B-Cell Lymphoma of the Small Bowel in Female Patient Causing Intestinal Obstruction: A Case Report
Andrej Nikolovski
Department of Visceral Surgery, University Surgery Clinic “Sv. Naum Ohridski”, Medical Faculty, Skopje, North Macedonia
E-mail: andrejnikolovski05@gmail.com
ORCID: https://orcid.org/0000-0002-5286-3532
Sanja Trajkova
University Clinic for Hematology, Clinical Center “Mother Theresa”, Medical Faculty, Skopje, North Macedonia
E-mail: sanjatrajkovamd@yahoo.com
Dushko Dukovski
University Clinic for Hematology, Clinical Center “Mother Theresa”, Medical Faculty, Skopje, North Macedonia
E-mail: dule_mc@yahoo.com
Goran Spirov
University Institute of Positron Emission Tomography, Skopje, North Macedonia
E-mail: goranspirov@gmail.com
Gordana Petrushevska
Institute for Pathology, Medical Faculty, Skopje, North Macedonia
E-mail: gordanap61@yahoo.com
Abstract. Diffuse large B cell lymphoma is the most common extranodal non-Hodgkin lymphoma of the small intestine accounting for more than 50% of cases. Forty percent of these cases initially present with small bowel obstruction. Therefore, the diagnosis is usually established after surgery for bowel obstruction. The treatment is then continued with a certain chemotherapy regimens. We present a case of a 46-years-old female patient with signs of small bowel obstruction due to previously undiagnosed diffuse large B-cell lymphoma. Postoperatively, the patient was treated with 7 cycles of R-CHOP protocol and complete response was achieved in the short follow-up period.
Key words: diffuse large B-cell lymphoma, extranodal, small bowel obstruction.
Received: 2022/05/01. Accepted: 2022/06/24.
Copyright © 2022 Andrej Nikolovski, Sanja Trajkova, Dushko Dukovski, Goran Spirov, Gordana Petrushevska. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
The most frequent extranodal presentation of non-Hodgkin lymphoma (NHL) is the gastrointestinal tract (GIT), accounting for more than 30% of cases [1]. Additionally, diffuse large B-cell lymphoma (DLBCL) is the most common non-Hodgkin lymphoma and it is also frequently diagnosed with extranodal presentation in the gastrointestinal tract [2]. They are difficult to diagnose due to their insufficiently defined symptoms and the diagnosis is often established in an urgent settings [3]. The small intestine is the second most common place in GIT where extranodal NHL occurs (20% of all gastrointestinal lymphomas) [4]. Few reports in the literature exist on DLBCL causing acute small bowel obstruction [3, 5, 6]. We present a case of small bowel obstruction caused by an aggressive type of DLBCL in a female patient with previous absence of symptoms regarding malignant lymphoma. Written informed consent has been obtained from the patient.
Case presentation
A 46-years-old female patient presented to the emergency department with clinical signs of intestinal obstruction. The patient reported cramp and abdominal pain, and absence of flatus and stool passage one day prior to the exam. She had no previous abdominal surgery nor visible groin herniation on physical examination. The serum analysis showed C-reactive protein value of 5.80 (0.0–5.0 mg/L) and serum Iron level of 5.80 (6.6–28.3 μmol/L). Plain abdominal upright X-ray image confirmed the suspicion for intestinal obstruction (Figure 1).
Contrast-enhanced Computerized Tomography (CECT) of the abdomen was the next diagnostics tool. The small intestine was presented with dilated loops, formed “air fluid levels” and free fluid in the Douglas pouch. The tumor formation itself was not detected by the radiologist on this scan (Figure 2).
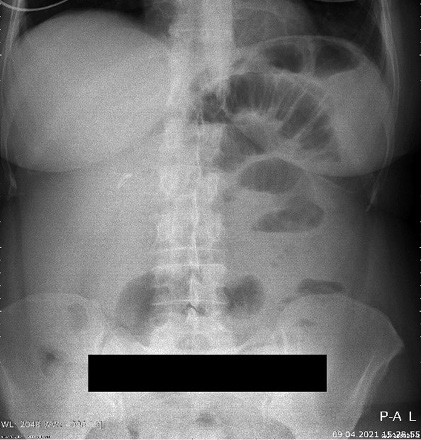
Figure 1. Plain abdominal X-ray with small bowel air-liquid levels

Figure 2. CECT of abdomen with signs of small bowel obstruction
Admission in hospital and exploratory laparotomy followed. Intraoperatively, a tumor with the size of an egg was found in the ileal wall causing the obstruction. Resection of the affected loop was done with a termino-terminal anastomosis. Postoperative period was uneventful and the patient was discharged on postoperative day 4. Superficial Surgical Site Infection (SSI) occurred at the first scheduled checkup and it was treated in the outpatient ward.
The macroscopic histopathology analysis revealed the presence of a tumor with dimensions of 6x5x2.5 cm (ulcerative type) that spreads in the surrounding adipose tissue. The microscopic aspect of hematoxylin and eosin staining presented with infiltrative growth of lymphoid cells with large nuclei and frequent mitoses. Immunohistochemical staining showed high proliferation over 90% of Ki67 and CD20 (Figures 3a, 3b, and 3c). The overall pathology report concluded the presence of aggressive diffuse large B-cell lymphoma.
3a 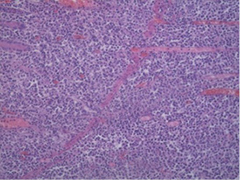 3b
3b 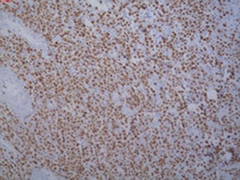 3c
3c 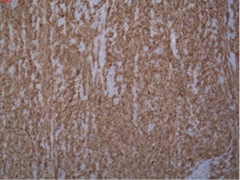
Figure 3. 3a – Hematoxylin Eosin stain with infiltrative growth of Lymphocytes, 3b – Ki67 stain with high proliferation, 3c – CD20 stain with proliferation over 90% (100x magnification)
The patient was referred to a hematologist for proper staging and therapy. The positron emission tomography-computed tomography (PET/CT) scan showed a normal findings with low metabolic activity in the area of the wound infection (Figure 4). Bone marrow biopsy was negative. According to the Lugano score [7], the patient was diagnosed with Stage I of the disease.
Seven cycles of R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisolone) regimen were given to the patient as the first line of treatment. Post-chemotherapy PET/CT scan presented with normal findings. The patient is still in complete remission after the combined treatment with surgery and chemotherapy and regular future checkups are scheduled.
Discussion
DLBCL remains to be the most common extranodal NHL in the small intestine in 56.8% of patients [5]. More than two-thirds are diagnosed in Stage I/II (70.7%) [8], but nevertheless, initial presentation with small bowel obstruction is reported in 40% of them [9, 10]. However, only a few case reports are published [3, 6, 7, 11]. According to gender distribution, the male to female ratio is 2:1 [12]. The diagnosis is challenging in the emergency setting and it is often established postoperatively [3].

Figure 4. PET/CT scan with normal finding
In these patients, there is still a debate which treatment modality offers the best results regarding the complete remission. The proposed first-line regimen for extranodal gastrointestinal DLBCL is the use of CHOP or R-CHOP chemotherapy protocols. Most of the reports give a significant advantage of the rituximab addition to the CHOP protocol in terms of significantly greater overall survival and progression-free survival [13, 14].
Several studies have shown that the combination of surgery (first) followed by chemotherapy provides better survival benefit in patients with DLBCL [15, 16]. According to Zhang, the combination of surgery and R-CHOP offers significantly better event-free survival, better response rate, lower relapse rate, and higher overall survival rate, but without statistical significance in older patients [12]. Hwang reports 5-year survival rate of 86.4% in cases treated with surgery plus CHOP or R-CHOP [17].
To conclude, an emergency abdominal condition with clinical signs of bowel obstruction in a young and/or middle aged patients without previous abdominal surgery history should raise suspicion for extranodal GIT lymphoma. One of the reliable therapeutic options in such emergency setup is the combination of surgery and chemotherapy and one should expect a complete therapeutic response in such patients.
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
1. Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer 1972; 29(1): 252–260.
2. Rojek AE, Smith SM. Evolution of therapy for limited stage diffuse large B-cell lymphoma. Blood Cancer Journal 2022; 12(2). DOI: 10.1038/s41408-021-00596-z.
3. Facundo H, Manrique MEA. Primary Lymphoma in the Small Intestine: A Case Report and Literature Review. Revista Colombiana de Gastroenterologia 2017; 32(1): 65–71.
4. Ghimire P, Wu GY, Zhu L. Primary gastrointestinal lymphoma. World J Gastroenterol 2011; 17(6): 697–707. DOI: 10.3748/wjg.v17.i6.697.
5. Kuroda K, Lucia A. Small Bowel Obstruction as an Initial Presentation of Mesenteric Follicular Lymphoma: Case Report and Literature Review. Cureus 2022; 14(1): 3–7. DOI: 10.7759/cureus.21566.
6. Vien LP, Bains A, Yeung HM. Primary extranodal jejunal diffuse large B cell lymphoma as a diagnostic challenge for intractable emesis: a case report and review of literature. J Community Hosp Intern Med Perspect 2019; 9(6): 518–523. DOI: 10.1080/20009666.2019.1687115.
7. Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E, Lister TA, Alliance, Australasian Leukaemia and Lymphoma Group; Eastern Cooperative Oncology Group; European Mantle Cell Lymphoma Consortium; Italian Lymphoma Foundation; European Organisation for Research; Treatment of Cancer/Dutch Hemato-Oncology Group; Grupo Español de Médula Ósea; German High-Grade Lymphoma Study Group; German Hodgkin’s Study Group; Japanese Lymphorra Study Group; Lymphoma Study Association; NCIC Clinical Trials Group; Nordic Lymphoma Study Group; Southwest Oncology Group; United Kingdom National Cancer Research Institute. Recommendations for Initial Evaluation, Staging, and Response Assessment of Hodgkin and Non-Hodgkin Lymphoma: The Lugano Classification. J Clin Oncol 2014; 32(27): 3059–3068. DOI: 10.1200/JCO.2013.54.8800.
8. Wang M, Ma S, Shi W, Zhang Y, Luo S, Hu Y. Surgery shows survival benefit in patients with primary intestinal diffuse large B-cell lymphoma: A population-based study. Cancer Med 2021; 10(10): 3474–3485. DOI: 10.1002/cam4.3882.
9. Matysiak-Budnik T, Jamet P, Fabiani B, Nion-Larmurier I, Marjanovic Z, Ruskoné-Fourmestraux A, Groupe D’étude des Lymphomes Digestifs (GELD), Federation Francophone de Cancerologie Digestive (FFCD), Dijon, France. Primary intestinal B-cell lymphoma: a prospective multicentre clinical study of 91 cases. Dig Liver Dis 2013; 45(11): 947–952. DOI: 10.1016/j.dld.2013.05.008.
10. Malipatel R, Patil M, Rout P, Correa M, Devarbhavi H. Primary Intestinal Lymphoma: Clinicopathological Characteristics of 55 Patients. Euroasian J Hepatogastroenterol 2021; 11(2): 71–75.
11. Sharma KD, Massey AV, Vijayvargiya M, Jain S. A case of multiple recurrent intussusceptions due to multiple lymphomatous polyposis associated with diffuse large B-cell lymphoma of gastrointestinal tract in a 15-year-old child: A rare case report. Int J Surg Case Rep 2021; 79: 44–48. DOI: 10.1016/j.ijscr.2020.12.061.
12. Zhang L, Huang H, Wang Z, Fang X, Hong H, Chen Y, Li F, Yao Y, Chen Z, Pan F, Li X, Chen M, Gale RP, Liang Y, Lin T. Surgery and Chemotherapy versus Chemotherapy Only in Older Persons with Primary Intestinal Diffuse Large B-Cell Lymphoma. Cancer Manag Res 2021; 13: 8831–8839.
13. Li X, Shen W, Cao J, Wang J, Chen F, Wang C, Zou S, Shen B, Zhao R, Li J, Shen Z. Treatment of gastrointestinal diffuse large B cell lymphoma in China: a 10-year retrospective study of 114 cases. Ann Hematol 2012; 91(11): 1721–1729. DOI: 10.1007/s00277-012-1507-1.
14. Sunggoro AJ, Dwianingsih EK, Utomo BP, Purwanto I. A Complicated Case of Diffuse Large B-Cell Lymphoma in an Elderly Presenting with Massive Gastrointestinal Bleeding Successfully Treated with R-mini CHOP. Case Rep Oncol 2021; 14(1): 262–268. DOI: 10.1159/000512826.
15. Ibrahim EM, Ezzat AA, El-Weshi AN, Martin JM, Khafaga YM, Al Rabih W, Ajarim DS, Al-Foudeh MO, Zucca E. Primary intestinal diffuse large B-cell non-Hodgkin’s lymphoma: clinical features, management, and prognosis of 66 patients. Ann Oncol 2001; 12(1): 53–58. DOI: 10.1023/a:1008389001990.
16. Kim SJ, Kang HJ, Kim JS, Oh SY, Choi CW, Lee SI, Won JH, Kim MK, Kwon JH, Mun YC, Kwak JY, Kwon JM, Hwang IG, Kim HJ, Park J, Oh S, Huh J, Ko YH, Suh C, Kim WS. Comparison of treatment strategies for patients with intestinal diffuse large B-cell lymphoma: surgical resection followed by chemotherapy versus chemotherapy alone. Blood 2011; 117(6): 1958–1965. DOI: 10.1182/blood-2010-06-288480.
17. Hwang HS, Yoon DH, Suh C, Park CS, Huh J. Intestinal diffuse large B-cell lymphoma: an evaluation of different staging systems. J Korean Med Sci 2014; 29(1): 53–60. DOI: 10.3346/jkms.2014.29.1.53.