Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2023, vol. 22(4), pp. 234–237 DOI: https://doi.org/10.15388/LietChirur.2023.22(4).5
A Rare Case of Parotid Tuberculosis in a Pediatric Patient: A Case Report
Aditya Pawar
Department of Surgery, Armed Forces Medical College, Pune, India
E-mail: suryaditya05@gmail.com
Niranjan Sahoo
Department of Pediatrics, Military Hospital, Bhopal, Madhya Pradesh, India
E-mail: niranjan.sahoo@gmail.com
Pawan Sharma
Department of Surgery, Armed Forces Medical College, Pune, India
E-mail: pawan.sharma@gmail.com
Nidhi Rathi
Department of Pathology, Military Hospital, Bhopal, Madhya Pradesh, India
E-mail: nidhi.rathi@yahoo.com
Abstract. Even in countries like India where the general dictum is to consider Tuberculosis as one of the differential diagnosis to any condition that is still under evaluation. Parotid Tuberculosis is a very rare entity. There are fewer than 200 cases reported in literature worldwide of Parotid gland Tuberculosis, a form of extrapulmonary Tuberculosis. We present an interesting case of Parotid Tuberculosis which presented as unilateral swelling in the parotid region of a four-year-old male child with an underlying abscess.
Keywords: parotid, tuberculosis, extra pulmonary tuberculosis.
Received: 2023/05/02. Accepted: 2023/06/30.
Copyright © 2023 Aditya Pawar, Niranjan Sahoo, Pawan Sharma, Nidhi Rathi. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
This case report throws light on a very interesting facet of Extra Pulmonary Tuberculosis. Parotid Tuberculosis is a very rare presentation of EPTB and even in country like India which shares the majority burden of TB and it’s varied presentation, a case of Parotid Tuberculosis is a rarity. This fact is emphasised by the fact that the there are only about 200 odd cases reported in literature on the topic. What makes our case report even more interesting is the age group of our patient, a 4-year-old male child. The literature on paediatric parotid tuberculosis is even more obscure.
Case Presentation
A 4-year-old male child presented with gradually increasing swelling in the right parotid region and right side of neck of 10 days duration (Figure 1), associated with mild pain and difficulty in swallowing. There was history of fever for 2 days preceding the onset of swelling. There was no history of rash, cough, testicular pain, trauma, or any complaints on the contralateral parotid region. There was no history of constitutional symptoms like malaise, low grade fever, anorexia, weight loss. There was no history of contact with any tuberculosis patients.
On physical examination, the patient, was average built, and his weight was within normal limit for his age. He had mild pallor. On local examination of the swelling, a well-defined unilateral mass of 6×5 cm was found, obliterating the right angle of jaw. It was firm, compressible swelling, mobile in vertical plane, nontender with smooth skin surface. Local temperature was not raised and had no discharging sinus. Multiple right sided, matted, mobile cervical lymph nodes were palpable which were firm in consistency, largest measuring 4×2 cm in size at Right submandibular region. Few sub centimetric lymph nodes were palpable on left cervical region. Left side angle of jaw was normal, with no lymphadenopathy appreciated in any other region.
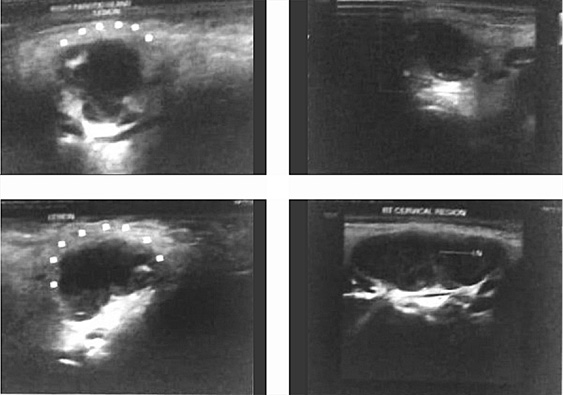
Routine blood investigations revealed haemoglobin 10.7 g/dl and total leucocyte count 15900/cumm with 55% neutrophils and 40% lymphocytes. ESR was 28 mm/hr. Ultrasonography of the swelling revealed intra-parotid collection measuring 21x17x18 mm in the superficial lobe with debris, suggestive of abscess (Figure 2). It also showed multiple matted lymph nodes bilaterally (RT > LT), largest one measuring 39x21 mm, level-Ib (RT). A CT scan neck was not done in order to circumvent exposure to high radiation and also due to it’s poor specificity in differentiating tuberculosis from neoplastic lesions. FNAC was performed, and 3 ml pus was aspirated, which showed epithelioid granulomatous cells in the background of acute inflammatory exudates (Figure 3). Tuberculin test was highly positive at 18 mm. Chest X-ray was normal. The patient was started on Anti-Tuberculosis Therapy (ATT), with 4 drugs, i.e., Rifampicin, Isoniazid, Pyrazinamide, and Ethambutol for 2 months, followed by Rifampicin and Isoniazid for next 4 months. On follow-up after 15 days, swelling size had reduced significantly following spontaneous burst open of the swelling. The wound was expressed, cleaned and dressed regularly. The patient is on regular follow up and started gaining weight with healing of the rupture site.
|
Figure 1 |
Figure 2 |
|
Figure 3 |
Discussion
As per the WHO report 9.9 million fell ill with Tuberculosis in the year 2020 and a whooping 1.5 million people died from the disease. India continues to figure in the list of countries that top the high burden criteria of WHO. As per the Global TB Report published as recently as Oct 2022, India has figured in the top 20 list of countries with High TB Burden, High TB with HIV burden and the High MDR/RR TB burden countries [1]. TB has primary propensity to involve lungs via aerosol transmission being an infectious disease but has shown to any involve any organ system via hematogenous or lymphatic channels which is termed as Extra Pulmonary Tuberculosis (EPTB) [2, 3]. Indian data suggests that the burden of EPTB is high ranging from 15–20% in HIV negative cases and ranging from 40–50% of the freshly detected cases in HIV positive population [4]. The estimated incidence of all forms of TB reported for the year 2020 is 188 per 1,00,000 population. The total number of incident TB patients (new & relapse) notified during 2021 was 19,33,381 which was 19% higher than that of 2020 (16,28,161), indicating a recovery noted in reporting following dip noted during COVID-19 [5].
EPTB includes a wide variety of system involvement, most common ones are tuberculosis of lymph nodes, pleura, skeletal, meninges, abdominal, genito-urinary and pericardial [6, 7]. Parotid Tuberculosis is a very rare variety of EPTB, with only around 200 odd cases reported in literature worldwide [8]. C. De Paoli reported the first case of parotid gland tuberculosis in 1893 [9]. Parotid are physiologically a difficult site to be affected by TB due to presence of thiocyanate ions and proteolytic activity of salivary enzymes, also their regular flow prevents stagnation [10].
Tuberculosis reaches parotids usually as a secondary infection and the main routes of transmission are from oro-pharyngeal cavity by the retrograde transmission via Stenson’s ducts [11]. Other rarer mode of transmission is via hematogenous or lymphatic spread [12]. They usually present as slow growing unilateral swelling, however they may vary from an acute presentation to a chronic indolent swelling. In our case it was an acute presentation with a history of just 10 days. The evaluation of a unilateral parotid swelling entails differentiating it from benign swellings like parotid cyst following ductal lithiasis, parotitis, adenitis, benign tumour or rarely malignant growth. Being a superficial lesion, they are very amenable to ultrasonography. Sonography can help us differentiating it into two subgroups i.e. parenchymal or peri-parotid type depending on the location [7]. However the radiological investigation like Ultrasonography, CT and MRI may be helpful in delineating the location and the extent of the disease but the findings are not specific, and hence many findings mimic neoplasm [13]. A chest X-ray is essential to rule out any primary focus. A metanalysis done on 49 cases confirmed a primary lung focus in 25% cases [14]. It is thus not wise to base decisions on clinical and radiological inputs only as it can lead to inadvertent surgery which was the case couple of decades earlier where most of the diagnosis of parotid tuberculosis were made from hist-pathological examination, post-operatively [10]. FNAC has thus evolved as an inevitable step in evaluation of Parotid swellings with an impressive sensitivity (81%–100%) as well as specificity (94%–100%) [15]. However, a non-conclusive FNAC can be investigative dead end and thus many authors do recommend Polymerase Chain Reaction to increase the positive cyto-culture results. We find ourselves lucky as the FNAC done on our patient could yield epithelioid granulomatous cells and patient could be started on Antituberculosis Treatment (ATT). The four-drug treatment based on Isoniazid (H), Rifampicin (R), Pyrazinamide (Z) and Ethambutol (E) in intensive phase of two months and two drugs H & R in continuation phase for four months was currently used as advised for EPTB of lymph nodes and abdominal TB, however there were no guidelines given specifically for Parotid EPTB by the taskforce formed to draft guidelines on the evaluation and management of EPTB in India [16].
We conclude by saying that Parotid Tuberculosis should be kept as a rare but important differential guided by clinical suspicion and should be evaluated thoroughly to prevent mis-diagnosing this medically manageable entity and thus prevent unnecessary surgical intervention and it’s possible complications.
Acknowledgement
We would like to express gratitude towards Dr. Ajay Jain and Dr. Shweta Goyal for first evaluating the patient. Dr. Richa Gupta who provided us with the first radiological impression, Dr. Rashmi Nichalani and Dr. Nidhi Rathi for their cytological opinions and lastly the child and his parents for their permission and co-operation.
References
1. Global Tuberculosis Report 2022. Geneva: World Health Organization, 2022. Licence: CC BY-NC-SA 3.0 IGO.
2. Fanning A. Tuberculosis: Extrapulmonary Disease. CMAJ 1999; 160(11): 1597–1603.
3. Iscman MD. Tuberculosis in Relation to Human Immunodeficiency Virus and Acquired Immunodeficiency Syndrome. In: Iseman MD, editor. A Clinician’s Guide to Tuberculosis. Philadelphia: Lippincott Williams and Wilkins, 2000, p. 199–252.
4. Sharma SK, Mohan A. Extrapulmonary Tuberculosis. Indian J Med Res 2004; 120(4): 316–353.
5. Glaziou P, Dodd PJ, Dean A, Floyd K. Methods Used by WHO to Estimate the Global Burden of TB Disease. Geneva: World Health Organization, 2020. Available at: <https://www.who.int/tb/publications/global_report/TB20_Technical_Appendix_20201014.pdf>.
6. Farer LS, Lowell AM, Meader MP. Extra Pulmonary Tuberculosis in USA. Am J Epidemiol 1992; 109: 205–217.
7. Kushwaha RAS, Kant S, Verma SK, Sanjay, Mehra S. Isolated Metacarpal Bone Tuberculosis: A Case Report. Lung India 2008; 25(1): 17–19.
8. Verma RK, Kaushal D, Bal A, Panda NK. Primary Parotid Tuberculosis Mimicking Parotid Neoplasm: A Rare Case Report. SEAJCRR 2013; 2: 455–462.
9. Chaudhary S. Tuberculosis of the Salivary Glands. In: Norman JE, McGurk M, editors. Colour Atlas and Text of The Salivary Glands. London: Mosby-Wolfe, 1997, p. 337–339.
10. Dixit R, Gokhroo A, Verma S, Panjabi M. Parotid Gland Tuberculosis. Int J Mycobacteriol 2017; 6(3): 318–320.
11. Sikora AG, Rothstein SG, Garay KF, Spiegel R. Tuberculosis of the Head and Neck. In: Rom WN, Garay SM, editors. Tuberculosis. 2nd edition. Philadelphia: Lippincott Williams and Wilkins, 2004, p. 477–488.
12. Myer C, Cotton RT. Salivary Gland Disease in Children: A Review. Part 1: Acquired Non-Neoplastic Disease. Clin Pediatr (Phila) 1986; 25(6): 314–322.
13. Gupta V, Patankar K, Shinde A, Bhosale C, Tamhane A. Tuberculosis of the Parotid Gland. Case Rep Radiol 2012; 2012: 278793. DOI: 10.1155/2012/278793.
14. Lee IK, Liu JW. Tuberculous Parotitis: Case Report and Literature Review. Ann Otol Rhinol Laryngol 2005; 1 14(7): 547–551.
15. Iserì M, Aydyner O, Celìk I, Peker O. Tuberculosis of the Parotid Gland. J Laryngol Otol 2005; 119(4): 311–313. Available at: <http://dx.doi.org/10.1258/0022215054020494>.
16. World Health Organization. Treatment of Tuberculosis: Guidelines for National Programs. WHO/CDS/TB/2003.313. Geneva: WHO, 2003.
17. Sharma SK, Ryan H, Khaparde S, Sachdeva KS, Singh AD, Mohan A, Sarin R, Paramasivan CN, Kumar P, Nischal N, Khatiwada S, Garner P, Tharyan P. Index-TB Guidelines: Guidelines on Extrapulmonary Tuberculosis for India. Indian J Med Res 2017; 145(4): 448–463. DOI: 10.4103/ijmr.IJMR_1950_16.