Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2024, vol. 23(1), pp. 25–33 DOI: https://doi.org/10.15388/LietChirur.2024.23(1).9
Airway Management in Pan Facial Fracture: An Outcome Analysis of Elective Tracheostomy and Submental Endotracheal Intubation
Vipin Venugopal Nair
Department of Surgery, Armed Forces Medical College, Pune, India
E-mail: vipinvenugopalnair@gmail.com
ORCID: https://orcid.org/0000-0001-6903-6368
Yuvraj Issar
Department of Oral and Maxillofacial Surgery, Armed Forces Medical College, Pune, India
E-mail: yuvraj.issar189@gmail.com
ORCID: https://orchid.org/0000-0002-0236-4727
Harmanjot Singh Dhillon
Department of Anaesthesia, Armed Forces Medical College, Pune, India
E-mail: drharmandhillon@gmail.com
ORCID: https://orcid.org/0000-0001-8396-5980
Gurpinder Singh Ghotra
Department of Anaesthesia, Armed Forces Medical College, Pune, India
E-mail: gpsghotra5@gmail.com
ORCID: https://orcid.org/0000-0002-7944-0214
Pranay Pratap
Department of Plastic Surgery, Armed Forces Medical College, Pune, India
E-mail: pranaypratap2@gmail.com
ORCID: https://orcid.org/0000-0003-2502-5346
Ayush Mathur
Department of Surgery, Armed Forces Medical College, Pune, India
E-mail: drayushmathur16@gmail.com
ORCID: https://orcid.org/0009-0001-6856-4318
Kamalpreet Singh
Department of ENT, Armed Forces Medical College, Pune, India
E-mail: kpsingh_81@yahoo.com
ORCID: https://orcid.org/0000-0002-2998-0044
Abstract. Background and Aims. Pan facial fractures are complex and often requiring complex airway management. Elective tracheostomy (ET) and submental endotracheal intubation (SEI) are the two major techniques for airway management. The aim of this article is to compare the management outcome between these techniques. Methods. This study was done in a tertiary care hospital from Jan 2019 to Dec 2019. Data were retrieved for all patients from hospital admission-discharge reports, operation room records, follow-up notes, and clinical photograph records which was recorded prospectively after ethical clearance. Total 38 patients were included in the study after the exclusion criteria into two groups: submental endotracheal intubation (SEI) and elective tracheostomy (ET). Demographic data, intraoperative time (IOT), length of hospital stay (LOHS), postoperative pain score at three and seven days, and Vancouver Scar Score (VSS) at 4 and 12 weeks was compared between the two groups. Results. SEI consisted of 23 patients (60%) while ET had 15 (40%) patients. The mean age was 32.77±8.24 years in the SEI and 29.36±7.32 years in the ET. The IOT in SEI was 15.36±1.53 min and 24.60±1.40 min in the ET which was statistically significant (p = 0.00001). The LOHS was 11±3.87 days in SEI and 25.2±3.88 days in ET (p = 0.0001). The mean VSS at 4 and 12 weeks for SEI were moderate and mild respectively and for the ET was moderate and mild respectively. Both were statistically significant with a p = 0.003 and p = 0.006. Conclusion. Submental intubation is a safe airway management technique in pan facial fracture. It provides the surgeon with an excellent operative field for achieving the proper dental occlusion. Both short- and long-term outcomes are better compared to the alternative airway method of elective tracheostomy.
Keywords: pan facial fracture, submental endotracheal intubation, elective, tracheostomy, scar.
Received: 2023/11/30. Accepted: 2023/12/22.
Copyright © 2024 Vipin Venugopal Nair, Yuvraj Issar, Harmanjot Singh Dhillon, Gurpinder Singh Ghotra, Pranay Pratap, Ayush Mathur, Kamalpreet Singh. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Pan facial fractures (PFF) is a complex injury requiring multi-disciplinary management. PFF involves the fracture of the mandible, maxilla, and zygomatic complex at the same time. It is usually associated with naso-orbito-ethmoid (NOE) and frontal bone fractures. They are soft tissue injuries and loss of bony structures that can lead to severe post-traumatic deformities and disabilities. Primary airway management in these patients is complex and depends on many factors such as etiology, the extent of injury, GCS at presentation, and comorbidities [1, 2].
In all PFF patients with associated unstable facial fracture segments and severe head injury, emergency tracheostomy is vital to save a life. In the present-day scenario, elective tracheostomy (ET), as well as submental endotracheal intubation (SEI), are the two major techniques for airway management in PFF during elective surgery [3, 4]. This aim of this article is to estimate whether SEI is a better modality than ET in surgical airway management of PFF.
Methods
This retrospective analysis was done in a prospectively collected data from a tertiary care teaching hospital in Western India after ethical clearance. The ethical approval was obtained from the Institutional Ethics Committee for the conduct of the study. The study took place from Jan 2019 to Dec 2019. All patients of PFF reporting to the emergency department requiring surgical management were included in the study. The exclusion criteria were a) age less than 12 years, b) pregnant women, and c) emergency tracheostomy. Data were retrieved from hospital admission discharge reports, operation room records, patient follow-up notes, and clinical photograph records. All patients with PFF who underwent elective open reduction and internal fixation were grouped alternatively into two groups. The SEI Group consisted of all patients managed by oral submental intubation and the ET Group consisted of all patients with elective tracheostomy.
In all cases anaesthesia management and surgeries were done by faculty of same calibre and knowledge. All elective tracheostomies were performed using appropriately sized tracheostomy tubes. A horizontal incision was made two fingers length above the suprasternal notch in all cases. Strap muscles were separated, the thyroid isthmus was retracted and a tracheostomy tube was inserted by creating a tracheal window between the 2nd and 3rd tracheal rings. As part of the termination of mechanical ventilation, the tracheostomy was closed, and other associated injuries of the patient were also addressed.
In all cases of SEI, the patient is initially intubated normally through the oral route using an appropriate-sized flexometallic endotracheal tube (ETT). The patient is then attached to a mechanical ventilator with FiO2 of one. A small incision was made over the paramedian aspect of the oral floor from outside. The mylohyoid muscle is split using forceps, and a communication channel is made into the oral cavity through this wound. The proximal end of this ETT is disconnected and bought out through the submental incision. The disconnected proximal end of ETT is then connected back to the mechanical ventilator. Once the procedure is over the endotracheal tube is disconnected and removed. The incision site is closed using single-layer nylon sutures which were removed after five days.
The demographic data, mode of injury, intraoperative time (IOT), length of hospital stay (LOHS), and postoperative pain score were retrieved from hospital records. The pain was recorded as a visual analogue scale pain (VAS-Pain) score of 0–10 where 0 is no pain and 10 is maximum pain. Further VAS was categorized as mild (1–3), moderate (4–7) and severe (8–10). The VAS pain was evaluated on the third post-operative day and seventh postoperative day. The clinical photographic section provided follow-up images for comparing scar quality. The postoperative scare was evaluated using Vancouver Scar Score (VSS) at 4 weeks and 12 weeks.
All patients underwent elective surgery according to the Arbeitsgemeinschaft für Osteosynthesefragen (AO) protocol. The decision for SEI and ET was taken independently by the surgical team as per the expertise of the team. Our null hypothesis was that there is no difference between the intraoperative time and postoperative outcome when comparing ET to SEI. Data were entered in Microsoft Excel 365 version 16.53 and analysed with SPSS version 26 (IBM USA) for data with a normal distribution, Levene’s test of equity of variance was performed. Means of continuous variables are evaluated using Student’s t-test for statistical significance. Categorical data were analysed using Chi-square test. A statistical p-value <0.05 was taken as significant.
Results
After receiving institutional ethical committee approval, a total of 46 patients presenting with PFF were included in the study. We excluded eight patients because they underwent emergency tracheostomies. The mean age was 32.77±8.24 years in SEI and 29.36±7.32 years in the ET group. There were 23 patients in the SEI group (60%) and 15 patients in the ET group (40%) (Figure 1). There were four females (11%) and the rest were males (89%). Road traffic accidents were the most common type of injury (81% of 30). The other modes were falling from height 11% (n = 4), interpersonal violence (n = 2), and victim of landslide (n = 1) (Table 1). There were no associated injuries in 12 patients. The rest had a few minor injuries not affecting management outcomes.
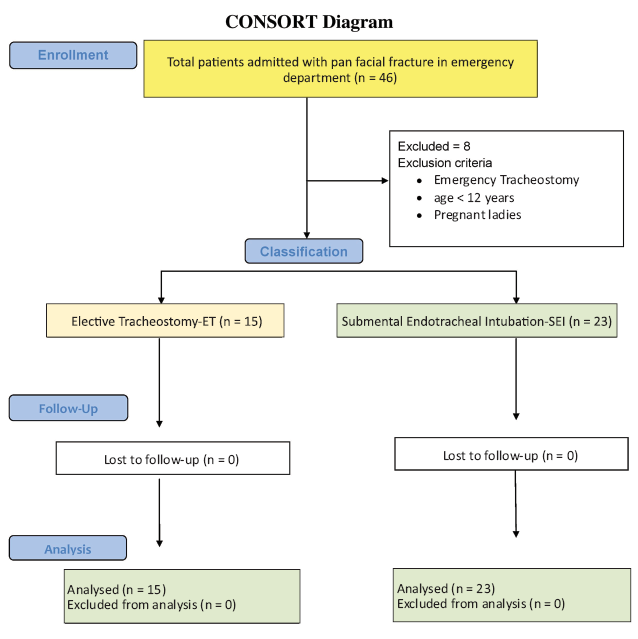
Figure 1. CONSORT diagram
Table 1. Demographic characteristics and study variables
|
Variables |
Submental Endotracheal |
Elective Tracheostomy |
p-Value |
|
|
Patients included (n) |
23 |
15 |
_ |
|
|
Sex |
M |
20 |
13 |
|
|
F |
3 |
2 |
||
|
Age (yrs) |
32.77±8.24 |
29.36±7.32 |
– |
|
|
Mode of Injury |
|
|
|
|
|
RTA |
19 |
12 |
||
|
Fall |
3 |
1 |
||
|
Landslide |
1 |
0 |
||
|
Interpersonal Violence |
0 |
2 |
||
|
Intraoperative Time (Min) |
15.36±1.53 |
24.60±1.40 |
<0.00001 |
|
|
LOHS* (Days) |
11.00±3.87 |
25.20±3.88 |
<0.00001 |
|
|
VAS# Pain (3 Days) |
5.73±1.20 |
NA |
NA |
|
|
VAS Pain (7 Days) |
1.48±1.16 |
1.27±0.82 |
0.300684 |
|
|
Mean VSS$ Score (4 Wks) |
3.45±1.26 |
4.87±1.64 |
0.00372 |
|
|
Mean VSS Score (12 Wks) |
0.41±0.59 |
1.00±0.85 |
0.006208 |
|
* Length of hospital stay, # Visual analog scale, $ Vancouver scar scale.
The IOT in SEI was 15.36±1.53 min and 24.60±1.40 min in the ET group which was statistically significant (p = 0.00001). The LOHS was 11±3.87 days in SEI and 25.2±3.88 days in ET with a significant result (p = 0.00001). The VAS score for pain at 3 days was moderate for SEI and could not be assessed in ET patients due to tracheostomy. Similarly, at seven days the VAS score was mild and for both SEI and ET and nonsignificant. The mean VSS at 4 and 12 weeks for SEI scar were moderate and mild respectively. Meanwhile, the mean VSS at 4 and 12 weeks for the ET was severe and moderate respectively. Both were statistically significant (p = 0.003 and p = 0.006) hence disproving the null hypothesis (Table 1). There was no major complication seen in either group except incision site abscess in one case of SEI on day 3. This was drained and left to heal by secondary intention. Two representative pictures each of SEI and ET from presentation to 12 weeks follow-up are shown in Figures 2–5.
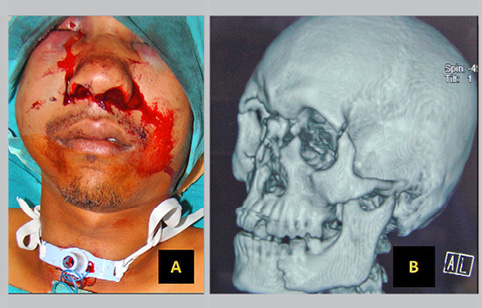

Figure 2. Elective tracheostomy group.
A – post-elective tracheostomy, B – NCCT with 3D reconstructive view of pan facial fracture, C – post-operative, D – post-operative 12 weeks.
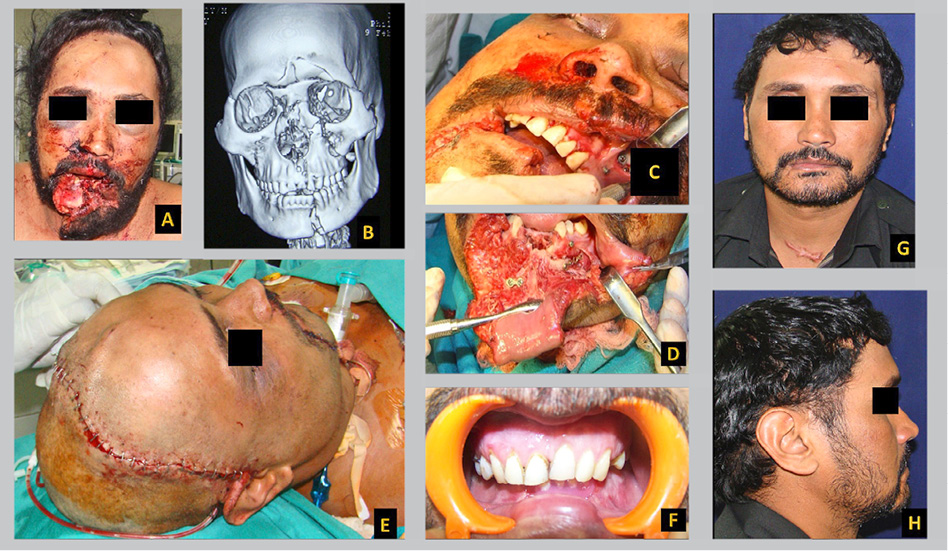
Figure 3. Elective tracheostomy group
A – pre-operative, B – NCCT with 3D reconstructive view of pan facial fracture, C – peri-operative, D – peri-operative, E – tracheostomy, F – dental occlusion achieved, G – post-operative 12 weeks hypertrophic tracheostomy scar, H – post-operative 12 weeks lateral view.
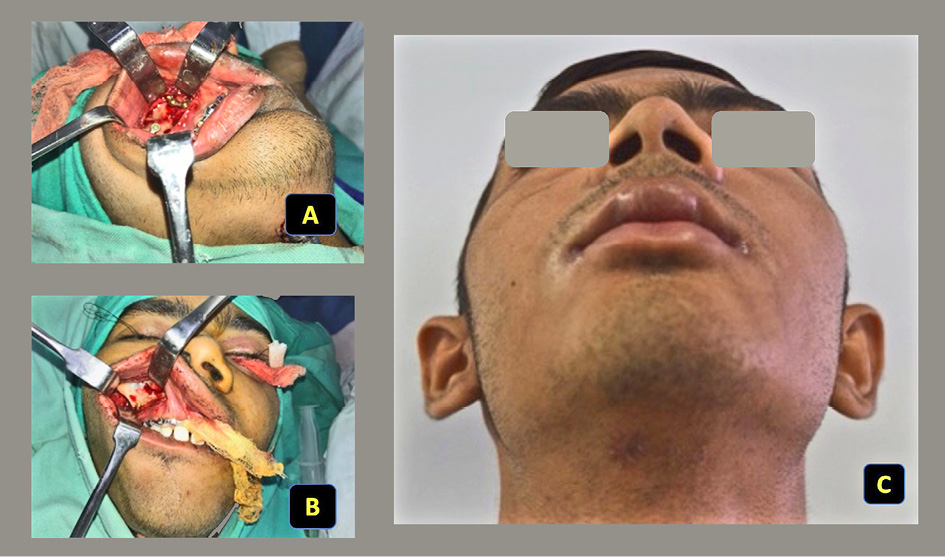
Figure 4. Elective submental intubation group
A – peri-operative picture with submental intubation, B – peri-operative oral malocclusion, C – post-operative scar 12 weeks.
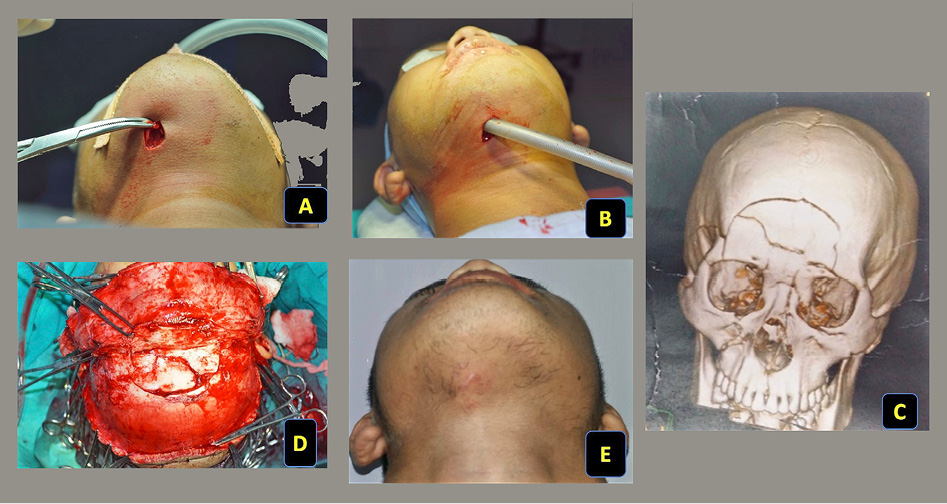
Figure 5. Elective submental intubation group
A – pre-operative submental incision, B – peri-operative submental intubation, C – NCCT with 3D reconstructive view of pan facial fracture, D – peri-operative fracture fixation, E –submental scar 12 weeks.
Discussion
When considering surgical fixation, airway management is an extremely crucial consideration. Nasal intubation is dangerous when the nose is fractured. The other option is oral intubation which can be performed safely. However, an endotracheal tube in the mouth prevents the surgeon from checking occlusion during various stages of surgery. Hence, the best available option for secure airway in these cases is performing a tracheostomy. Tracheostomy completely bypasses the upper airway thus facilitating a secure and safe airway for ventilation. However, tracheostomy is associated with many immediate problems like trans-tracheal dissection surgical emphysema, bleeding, and laryngeal nerve damage. The long-term complications involve tracheal stenosis, tracheoesophageal fistula, and many times scarring [5]. SEI originally described by Hernandez Altemir is another method, where an alternative route is established for tracheal intubation [6]. Here the proximal end of the endotracheal tube is diverted through the soft tissues of the submental region for elective ventilation. This type of intubation has the advantage of not interfering with the dental occlusion during surgery, avoiding the NOE area preventing accidental migration of the endotracheal tube into the cranial cavity or meningitis due to nasal instrumentation [7]. Gandhi et al. [8] clearly defined the critical indication of SEI as the patient in whom nasal intubation is contraindicated due to severity of the injury and otherwise doesn’t require tracheostomy but requires intra-operative maxillomandibular fixation during surgery.
Even though many papers have been written citing the advantage of this technique, there is still apprehension about using this method among many anaesthesiologists. This is proved by Lima et al. [9], who studied 3 149 patients over 10 years, of which 674 underwent general anaesthesia for surgical fixation of facial fractures. Only 15 patients underwent SEI. Similarly, Kaiser et al. [10] also found that SEI is a safe alternative for airways in PFF and is underutilized.
A study describing one of the largest series with 206 patients reported in India was published by Bhola and colleagues [11]. The average age was 31.61 years and 75% of the patients were males. The time required for SEI was 6±2 min. They concluded that in their experience, the anterior submandibular approach is a very reliable method with low morbidity. It is swift, easy, and has a small learning curve with minimal complications. Our study also showed male predominance with a mean age of 31.75±76 years which indicates that PFF is most commonly encountered in young males. A similar study in western literature by O’Connell et al. [12] further demonstrates the safety of the procedure and low complication rates. Schütz et al. [13] were also of the same opinion in their series of 222 patients. Caubi et al. [7] further conclude that SEI is a simple, secure, and effective procedure for airway control in PFF.
Emara et al. [14] compared the time required for the procedure and found that SEI is faster to perform than a tracheostomy. In the prospective study on 32 patients, they found that the average time for SEI was 8.35 min as opposed to 30.75 min for elective tracheostomy with a p = 0.0001. They also noted the postoperative scar was more cosmetically acceptable in SEI compared to ET with a p = 0.0325. In our study, the average time required for SEI was 15.36±1.53 which was nearly double the time required by the above study. The reason for the longer duration may be that the team is less experienced in performing SEI. However, the time for ET was comparable.
In their series of 288 patients with 45 SEIs, Gupta et al. [15] had a mean hospital stay of 16 days. Das et al. [16] also established the requirement of more days of hospitalization in ET patients. Similar results were reported by Mishra et al. [17] where the mean LOHS for SEI was 7 days. This is comparable to our results. In our study, the SEI patients were discharged earlier with a mean LOHS of 11 days. In contrast, the mean LOHS in the tracheostomy group was 25 days and was statistically significant. This was because the patients who underwent tracheostomy were having severe associated injuries and hence need more periods of mechanical ventilation and intensive care.
Szantyr et al. [18] have the largest documented study of SEI with 316 patients over 20 years for various indications including trauma, cosmetic, functional, and malignancy. They thought that SEI was successful in providing a comfortable and safe operating field without an endotracheal tube. However, there are minor complications in the form of wound infection in 12 (3.8%), transient salivary fistula in three (0.95%), and hypertrophic scarring in two (2.21%) patients. In our series, there was only one complication noticed at the end of 12 weeks. This was a stitch abscess in one of the patients of SEI which was drained on the fifth post-operative day. These were similar to most of the recent studies in the literature [7, 19].
Various studies are showing various modifications of SEI. In all these studies the basic philosophy is the same. They differ in the way they exit the ETT. Various transmyelohyoid modifications include strict median, paramedian or anterior retrosymphisis [20, 21]. Some variations exist in the technique of delivery of the ETT through the submental tunnel. Some modifications utilize the use of two tubes instead of a single ETT for reducing the time of disconnection of ETT during passage through the submental tunnel. Several of them, like Nyarady et al. [22], suggested basic mathematical simplifications for the procedure. No matter which technique they advocate, all of them reiterate the merits of SEI in preventing an unwanted tracheostomy [11, 23–26].
Another large meta-analysis sums up the discussion on this airway management argument in PFF. This largest series was analysed by Goh et al. [26] in their meta-analysis of all papers from 1986 to 2018 published in PubMed, Scopus, and Cochrane Databases. This study included 2 229 patients in more than 100 published articles. The study concluded that the most common cause for SEI was trauma (81%). The preferred tube was a reinforced ETT and the paramedian route was preferred by 52% of anaesthesiologists. The mean surgical time was 10 min and there were 7% complications, mostly in the form of superficial skin infection. They also concluded that SEI is a safe and faster procedure with minimal complication and needs to be practiced more often [26].
Data from only one institution and a limited number of patients limit our study. It was not possible to assess pain in tracheostomized patients immediately following surgery by using a visual analogue score. Researchers found that the SEI works well in our population and can produce better patient outcomes. In this article, we attempts to sensitize the younger generation of anaesthesiologists to the importance of understanding the basics of this technique. We also recommend incorporating SEI into routine practice for better patient care.
Conclusion
Airway control in the management of pan facial fracture must be accorded the highest priority. The threshold for performing a tracheostomy in emergency airway management in pan facial fractures should be kept low. Submental intubation is a safe elective airway management technique. In the case of pan facial fracture apart from providing a safe airway, it also provides the surgeon with an excellent operative field to achieve appropriate dental occlusion. However, the technique is not widely used. The short-term and long-term outcomes are superior to elective tracheostomy. The method is easy to master and requires less time. This technique needs to be incorporated more frequently into our routine practice.
References
1. Venugopal MG, Sinha R, Menon PS, Chattopadhyay PK, Roy Chowdhury SK. Fractures in the maxillofacial region: a four year retrospective study. Med J Armed Forces India 2010; 66(1): 14–17.
2. Shetty PM, Yadav SK, Upadya M. Submental intubation in patients with panfacial fractures: a prospective study. Indian J Anaesth 2011; 55(3): 299–304.
3. Jundt JS, Cattano D, Hagberg CA, Wilson JW. Submental intubation: a literature review. Int J Oral Maxillofac Surg 2012; 41(1): 46–54.
4. Kar C, Mukherjee S. Submental intubation: an alternative and cost-effective technique for complex maxillofacial surgeries. J Maxillofac Oral Surg 2010; 9(3): 266–269.
5. Taicher S, Givol N, Peleg M, Ardekian L. Changing indications for tracheostomy in maxillofacial trauma. J Oral Maxillofac Surg 1996; 54(3): 292–295.
6. Hernández Altemir F. The submental route for endotracheal intubation. A new technique. J Maxillofac Surg 1986; 14(1): 64–65.
7. Caubi AF, Vasconcelos BC, Vasconcellos RJ, de Morais HH, Rocha NS. Submental intubation in oral maxillofacial surgery: review of the literature and analysis of 13 cases. Med Oral Patol Oral Cir Bucal 2008; 13(3): e197–e200.
8. Gandhi M, Ved BK. Submental intubation: a new approach in panfacial trauma. J Indian Med Assoc 2014; 112(1): 54–55.
9. Lima SM Jr, Asprino L, Moreira RW, de Moraes M. A retrospective analysis of submental intubation in maxillofacial trauma patients. J Oral Maxillofac Surg 2011; 69(7): 2001–2005.
10. Kaiser A, Semanoff A, Christensen L, Sadoff R, DiGiacomo JC. Submental intubation: an underutilized technique for airway management in patients with panfacial trauma. J Craniofac Surg 2018; 29(5): 1349–1351.
11. Bhola N, Jadhav A, Kala A, Deshmukh R, Bhutekar U, Prasad GSV. Anterior submandibular approach for transmyelohyoid endotracheal intubation: a reappraisal with prospective study in 206 cases of craniomaxillofacial fractures. Craniomaxillofac Trauma Reconstr 2017; 10(4): 255–262.
12. O’Connell JE, Kearns GJ. Submental intubation: a retrospective review of 45 cases. Ir J Med Sci 2013; 182(3): 309–313.
13. Schütz P, Hamed HH. Submental intubation versus tracheostomy in maxillofacial trauma patients. J Oral Maxillofac Surg 2008; 66(7): 1404–1409.
14. Emara TA, El-Anwar MW, Omara TA, Anany A, Elawa IA, Rabea MM. Submental intubation versus tracheostomy in maxillofacial fractures. Oral Maxillofac Surg 2019; 23(3): 337–341.
15. Gupta B, Prasad A, Ramchandani S, Singhal M, Mathur P. Facing the airway challenges in maxillofacial trauma: a retrospective review of 288 cases at a level i trauma center. Anesth Essays Res 2015; 9(1): 44–50.
16. Das S, Das TP, Ghosh PS. Submental intubation: a journey over the last 25 years. J Anaesthesiol Clin Pharmacol 2012; 28(3): 291–303.
17. Mishra R, Yadav D, Tripathi S, Kandel L, Baral PP, Shubham S, Karn A, Dutta K. Submental intubations in panfacial fractures. Clin Cosmet Investig Dent 2020; 12: 41–48.
18. Szantyr A, Szuta M, Zapała J. Airway management using submental intubation in head and neck surgery. Folia Med Cracov 2016; 56(3): 79–85.
19. Rodrigues WC, de Melo WM, de Almeida RS, Pardo-Kaba SC, Sonoda CK, Shinohara EH. Submental intubation in cases of panfacial fractures: a retrospective study. Anesth Prog 2017; 64(3): 153–161.
20. Oshima N, Shiraishi T, Kawauchi T, Oba J, Sato D, Fujiki M, Ozaki M, Takushima A, Harii K. A simple and reliable submental intubation technique for maxillofacial fractures. J Craniofac Surg 2018; 29(7): 1952–1955.
21. Mahmood S, Lello GE. Oral endotracheal intubation: median submental (retrogenial) approach. J Oral Maxillofac Surg 2002; 60(4): 473–474.
22. Nyárády Z, Sári F, Olasz L, Nyárády J. Submental endotracheal intubation in concurrent orthognathic surgery: a technical note. J Craniomaxillofac Surg 2006; 34(6): 362–365.
23. Chandu A, Smith AC, Gebert R. Submental intubation: an alternative to short-term tracheostomy. Anaesth Intensive Care 2000; 28(2): 193–195.
24. Biglioli F, Mortini P, Goisis M, Bardazzi A, Boari N. Submental orotracheal intubation: an alternative to tracheotomy in transfacial cranial base surgery. Skull Base 2003; 13(4): 189–195.
25. Taglialatela Scafati C, Maio G, Aliberti F, Taglialatela Scafati S, Grimaldi PL. Submento-submandibular intubation: is the subperiosteal passage essential? Experience in 107 consecutive cases. Br J Oral Maxillofac Surg 2006; 44: 12–14.
26. Goh EZ, Loh NHW, Loh JSP. Submental intubation in oral and maxillofacial surgery: a systematic review 1986–2018. Br J Oral Maxillofac Surg 2020; 58(1): 43–50.