Lietuvos chirurgija ISSN 1392–0995 eISSN 1648–9942
2023, vol. 22(3), pp. 179–184 DOI: https://doi.org/10.15388/LietChirur.2023.22(3).8
Hepatic Angiomyolipoma: A Case Report and Review of the Literature
Jekaterina Strelčenko
General and Abdominal Surgery and Oncology Department, National Cancer Institute, Vilnius, Lithuania
E-mail: jekaterina.strelcenko@gmail.com
Justas Kuliavas
General and Abdominal Surgery and Oncology Department, National Cancer Institute, Vilnius, Lithuania
E-mail: justas.kuliavas@gmail.com
Eugenijus Stratilatovas
General and Abdominal Surgery and Oncology Department, National Cancer Institute, Vilnius, Lithuania
E-mail: eugenijus.stratilatovas@nvi.lt
Audrius Dulskas
General and Abdominal Surgery and Oncology Department, National Cancer Institute, Vilnius, Lithuania
Department of Surgical Oncology, National Cancer Institute, Vilnius, Lithuania
E-mail: audrius.dulskas@gmail.com
Abstract. Background. Hepatic angiomyolipomas are uncommon non-cancerous mesenchymal tumors that belong to the perivascular epithelioid cell tumour group. Smooth muscle cells, fat cells and blood vessels can be observed in these types of neoplasm. Case presentation. We present the case of a 50-year-old patient. The patient was referred to the National Cancer Institute after an abdominal ultrasound, which incidentally revealed a mass in the liver. A whole body computed tomography scan showed a large liver mass, in the VII/VIII/V/VI segments. Trisegmenthomy of the right liver lobe was performed. Pathological examination revealed a rare, but benign tumour – angiomyolipoma. The postoperative course was uneventful and the patient was discharged on postoperative day 9. Two months following the surgery, the patient has no recurrence or late complications. Conclusion. Hepatic angiomyolipoma is a rare, usually benign tumour with malignant potential. It is can be diagnosed by radiological tests, biopsy or after surgery. The most common treatment is surgical resection.
Key words: hepatic angiomyolipoma, tumour, resection.
Kepenų angiomiolipoma: klinikinis atvejis ir literatūros apžvalga
Santrauka. Įvadas. Kepenų angiomiolipomos yra gana reti, dažniausiai gerybiniai navikai, priklausantys epitelioidinių ląstelių navikų grupei. Šio tipo navikus sudaro lygiųjų raumenų ir riebalinės ląstelės bei kraujagyslės. Klinikinio atvejo pristatymas. Straipsnyje aptariamas 50 m. paciento atvejis. Pacientas atsiųstas į Nacionalinį vėžio institutą atlikus ultragarsinį pilvo tyrimą, kurio metu atsitiktinai aptiktas darinys kepenyse. Atlikus viso kūno kompiuterinės tomografijos tyrimą, VII/VIII/V/V/VI segmentuose nustatytas didelis kepenų darinys. Atlikta dešiniosios kepenų skilties trisegmentomija. Patologinis tyrimas atskleidė esant retą gerybinį naviką – angiomiolipomą. Pooperacinė eiga buvo sklandi, devintą pooperacinę dieną pacientas išleistas gydytis ambulatoriškai. Po operacijos praėjus dviem mėnesiams pacientui nepasireiškė jokių recidyvų ar vėlyvųjų komplikacijų. Išvada. Kepenų angiomiolipoma yra retas, įprastai gerybinis navikas, kurio eiga gali būti piktybinio pobūdžio. Angiomiolipomą galima diagnozuoti radiologiniais tyrimais, atlikus biopsiją ar operaciją. Dažniausiai taikomas gydymas – chirurginė rezekcija.
Reikšminiai žodžiai: kepenų angiomiolipoma, navikas, rezekcija.
Received: 2023/08/01. Accepted: 2023/08/30.
Copyright © 2023 Jekaterina Strelčenko, Justas Kuliavas, Eugenijus Stratilatovas, Audrius Dulskas. Published by Vilnius University Press. This is an Open Access article distributed under the terms of the Creative Commons Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Introduction
Hepatic angiomyolipoma is a rare benign tumour of mesenchymal origin, that can potentially exhibit an aggressive clinical behavior. Although hepatic angiomyolipoma is classified as a benign tumour, there have been a few cases where the tumour has been identified as malignant [1, 2]. Most often, angiomyolipomas are composed of smooth muscle cells, adipose tissue, and blood vessels [3, 4]. However, the proportion and patterns of the tissues varies significantly from tumour to tumour and within the same tumour [5]. Depending on the ratio of the dominant tissue, tumours can be classified as lipomatous, myomatous, angiomatous or mixed. Mixed is the most common of these types [6]. Hepatic angiomyolipoma is more common in women and is usually found in the non-cirrhotic liver [7, 8]. However, several cases have also been reported among men [9].
With the increased use of imaging studies, most cases of angiomyolipomas are now discovered incidentally [10]. The most common site of involvement of this tumour is kidney, with the liver being the second most frequently involved organ [11]. The pathogenesis of this disease remains unclear, nevertheless an association with tuberous sclerosis complex has been observed in more than 50% of patients with renal angiomyolipoma, compared to only 10% of patients with hepatic angiomyolipoma [7]. The exact prevalence of hepatic angiomyolipoma is unknown due to non-specific clinical symptoms or asymptomatic presentation [12]. Only less than 600 cases of hepatic angiomyolipoma have been diagnosed and discribed so far in the literature [9].
Here we present a large hepatic AMP in a young woman. The clinical, treatment and pathological difficulties are being discussed.
Case report
A 50-year-old female patient presented to a healthcare facility with a headache. The patient did not report any specific symptoms or complaints related to the abdomen. The patient underwent blood tests, a chest X-ray and an abdominal ultrasound.
All the laboratory tests were within normal ranges and liver functional tests: alanine aminotransferase (ALT) and aspartate aminotransferase (AST), were not altered.
On abdominal ultrasound, a mass of at least 10 cm in diameter was observed in the right lobe of the liver, on the diaphragmatic surface.
An abdominal computed tomography (CT) scan of the liver, diaphragmatic surface, subcapsularly in segments VII/VIII/V/VI, showed a large tumour up to 13×10×13 cm with fatty inclusions, hypervascularised internal structures and calcinates (Figure 1). Tumour was fed by hypertrophied branches of the right hepatic artery. The convex surface of the mass is in contact with the intrahepatic part of the inferior vena cava in the upper part, and is deformed by the branches of the right hepatic vein slightly below. The trunk of the portal vein and the right branch are intact. In segment VI, several low-density foci of up to 8 mm are visible. Intrahepatic bile ducts and common bile-prominent in the peripheral parts, nevertheless not dilated.
The multidisciplinary team decided to perform surgical removal of the tumour. On operation, a 13–14 cm diameter, soft tissue tumour of the right hepatic lobe was removed (Figure 2).
Macroscopically, a liver fragment with a neoplastic mass was visible, the tumour was tender, friable; the section was yellowish in colour due to numerous fatty inclusions.
Microscopic examination of the tumour revealed a neoplastic nodule in the liver with an inhomogeneous structure. Lipocytes and large round polygonal cells with abundant eosinophilic granular cytoplasm, rounded nuclei of variable size and uniform chromatin were observed. Furthermore there was no increased mitotic activity in this tumour. In addition to lipocytes and polygonal cells, the tumour also contained areas of extramedullary haematopoiesis.
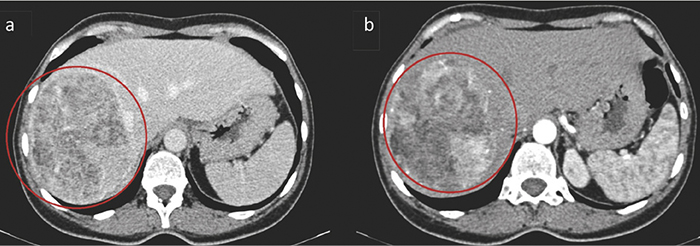
Figure 1. Hepatic angiomyolipoma in the right lobe of the liver (marked with red circle). A well-differentiated, circumscribed formation with uneven density due to fat and a denser soft tissue component (a). In the arterial phase, the part of the tumour without fat accumulates contrast (b)
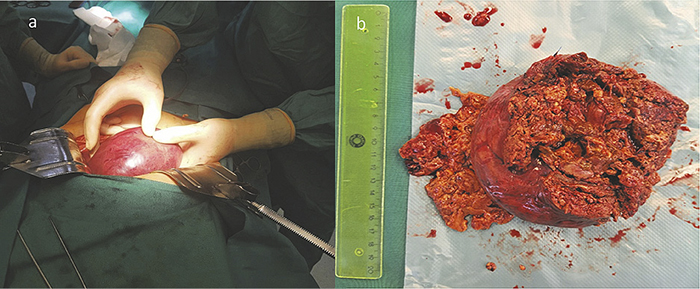
Figure 2. Intraoperative view of the tumour of the right liver lobe (a). Macroscopic view of a resected hepatic angiomyolipoma: 13–14 cm diameter, a soft tissue tumour of the right liver lobe was removed (b)
Table 1. Immunohistochemical analysis results
|
Stain |
Result |
|
HMB45 |
Positive |
|
SMA |
Slightly positive |
|
S-100 |
Negative |
|
PanCK |
Negative |
|
Synaptophysin |
Negative |
Immunohistochemical analysis of the surgical specimens showed that the tumour cells were positive for HMB45 and parts of them for smooth muscle actin (SMA). However, the tumour cells were negative for S-100, PanCK and syntaptophysin (Table 1).
Two months following the surgery, the patient has no recurrence or late complications and continues to be monitored (Figure 3).
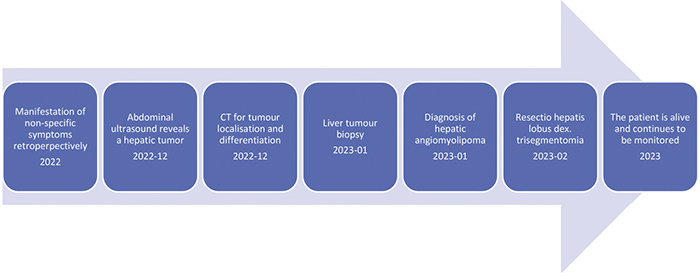
Figure 3. Timeline of presented case
Discussion
Most commonly, patients with hepatic angiomyolipoma do not have any specific complaints or clinical symptoms [12], as it was presented in our patient. Despite the fact that more than 50% of the cases have been found incidentally, unusual gastrointestinal symptoms such as nausea, vomiting, abdominal pain and discomfort were observed in several patients with hepatic angiomyolipoma [13].
Although hepatic angiomyolipoma has a very variable appearance on radiological imaging due to the different proportions of its constituent tissues and can easily be misdiagnosed as hepatocellular carcinoma or adenoma, especially when the tumour has a low lipid content [14]. This fact is also confirmed by the case of our patient, because the preliminary diagnosis that was made after radiological tests was liver adenoma. Diagnosing hepatic angiomyolipoma using only radiological examinations can be quite difficult, i.e. preoperative diagnosis is almost impossible due to the very different tissue proportion and the rarity of this type of tumour [15]. Notwithstanding the fact that CT scans and abdominal ultrasound may help in preoperative diagnosis, a thorough microscopic and immunohistochemical analysis is needed to confirm the diagnosis of hepatic angiomyolipoma [16]. Smooth muscle cells are the most specific marker for diagnosis, because the proportion of fat in a tumour can be extremely variable (from 10% to 70%) depending on the type of tumour: angiomatous, lipomatous, myomatous or mixed [6]. Smooth muscle cells can have a variety of morphologies and are positive for homatropin HMB45 and SMA, however negative for S100 protein [17, 18] (Table 1). In addition, according to some authors, if the tumour is radiologically similar to a hepatic angiomyolipoma and there is no clinical suspicion that it may be malignant, a fine needle aspiration biopsy (FNAB) followed by HMB45 staining may be performed to confirm preoperative diagnosis [18–20]. FNAB can be applied preoperatively to all patients without any clinical and serological abnormalities, but this diagnostic method is not recommended if surgical resection is necessary due to symptoms caused by the tumour [21].
The ideal course of treatment for hepaticangiomyolipoma remains debatable due to the small number of cases and lack of practical knowledge. If liver angiomyolipoma is accurately diagnosed before surgery, the tumour is asymptomatic and small (less than 5 cm) conservative treatment can be used [22]. The tumour can be monitored by radiological examinations during regular check-ups [21, 23]. However, as already mentioned, it is can be quite difficult to accurately diagnose hepatic angiomyolipoma by radiological imaging and hepatic FNAB is not always applicable [14, 15, 21]. Therefore, many researchers believe that surgical hepatic angiomyolipoma treatment by partial liver resection is the most effective and important method of treatment for all symptomatic or large tumours [12, 23]. In the case of our patient, the multidisciplinary team’s decision was to apply surgical treatment – resection of three segments of the liver.
In a systematic review by A. J. Klompenhouwer et al. [9], risk of mortality was around 0.8%. It is not high because hepatic angiomyolipomaL is generally a benign tumour and recurrence of the disease is rare [8, 9]. However, hepatic angiomyolipoma can sometimes demonstrate malignant characteristics, i.e. invasive growth, local recurrence and distant metastases after surgical treatment [1, 2, 9, 13]. In addition, complications of angiomyolipoma of the liver are not common. Nevertheless, due to its non-homogeneous appearance, sometimes a tumour in the liver can be inaccurately identified and pre-diagnosed as cancerous, with multiple foci, therefore not suitable for surgery and treated as malignant [24]. In some cases, hepatic angiomyolipoma can rupture and cause heavy bleeding, which can be fatal and needs to be treated urgently by embolisation or resection [10, 25].
Conclusion
Our study has several limitations – the most obvious – it is a case presentation. However, the strength of our paper is the thorough and comprehensive literature review.
To conclude, angiomyolipoma of the liver is a rare, however, possible differential diagnosis of liver tumours. Biopsy and radiological exam are needed. Surgical treatment is often performed for large symptomatic tumours.
References
1. Nguyen TT, Gorman B, Shields D, Goodman Z. Malignant Hepatic Angiomyolipoma: Report of a Case and Review of Literature. Am J Surg Pathol 2008; 32(5): 793–798. DOI: 10.1097/PAS.0b013e3181607349.
2. Deng YF, Lin Q, Zhang SH, Ling YM, He JK, Chen XF. Malignant Angiomyolipoma in the Liver: A Case Report with Pathological and Molecular Analysis. Pathol Res Pract 2008; 204(12): 911–918. DOI: 10.1016/j.prp.2008.06.007.
3. Limaiem F, Baccouch S, Boujelbene N, Atallah A, Hajri M, Gabsi S, Ben Farhat L, Bouraoui S. Puzzling Hepatic Tumor: Epithelioid Angiomyolipoma. Clin Case Rep 2022; 10(1): e05327. DOI: 10.1002/ccr3.5327.
4. Tsui WM, Colombari R, Portmann BC, Bonetti F, Thung SN, Ferrell LD, Nakanuma Y, Snover DC, Bioulac-Sage P, Dhillon AP. Hepatic Angiomyolipoma: A Clinicopathologic Study of 30 Cases and Delineation of Unusual Morphologic Variants. Am J Surg Pathol 1999; 23(1): 34–48. DOI: 10.1097/00000478-199901000-00004.
5. Nonomura A, Mizukami Y, Takayanagi N, Masuda S, Ishii K, Tashiro K, Mizoguchi Y. Immunohistochemical Study of Hepatic Angiomyolipoma. Pathology International 1996; 46(1): 24–32. DOI: 10.1111/j.1440-1827.1996.tb03529.x.
6. Seow J, McGill M, Wang W, Smith P, Goodwin M. Imaging Hepatic Angiomyolipomas: Key Features and Avoiding Errors. Clin Radiol 2020; 75(2): 88–99. DOI: 10.1016/j.crad.2019.09.135.
7. Klompenhouwer AJ, Dwarkasing RS, Doukas M, Pellegrino S, Vilgrain V, Paradis V, Soubrane O, Beane JD, Geller DA, Nalesnik MA, Tripke V, Lang H, Schmelzle M, Pratschke J, Schöning W, Beal E, Sun S, Pawlik TM, de Man RA, Ijzermans JNM. Hepatic Angiomyolipoma: An International Multicenter Analysis on Diagnosis, Management and Outcome. HPB 2020; 22(4): 622–629. DOI: 10.1016/j.hpb.2019.09.004.
8. Wang YJ, Wang YC, Chien CC, Chen CJ, Yang RN, Fang CL. Diagnosis of Hepatic Angiomyolipomata Using CT: Report of Three Cases and Review of the Literature. Clinical Radiology 2009; 64(3): 329–334. DOI: 10.1016/j.crad.2008.09.005.
9. Klompenhouwer AJ, Verver D, Janki S, Bramer WM, Doukas M, Dwarkasing RS, de Man RA, Ijzermans JNM. Management of Hepatic Angiomyolipoma: A Systematic Review. Liver Int 2017; 37(9): 1272–1280. DOI: 10.1111/liv.13381.
10. Kim SH, Kang TW, Lim K, Joh HS, Kang J, Sinn DH. A Case of Ruptured Hepatic Angiomyolipoma in a Young Male. Clin Mol Hepatol 2017; 23(2): 179–183. DOI: 10.3350/cmh.2016.0027.
11. Damaskos C, Garmpis N, Garmpi A, Nonni A, Sakellariou S, Margonis GA, Spartalis E, Schizas D, Andreatos N, Magkouti E, Grivas A, Kontzoglou K, Weiss MJ, Antoniou EA. Angiomyolipoma of the Liver: A Rare Benign Tumor Treated with a Laparoscopic Approach for the First Time. In Vivo 2017; 31(6): 1169–1173. DOI: 10.21873/invivo.11185.
12. Blokhin I, Chernina V, Menglibaev M, Kalinin D, Schima W, Karmazanovsky G. Giant Hepatic Angiomyolipoma: A Case Report. BJR Case Rep 2018; 5(1): 20180072. DOI: 10.1259/bjrcr.20180072.
13. Liu J, Zhang CW, Hong DF, Tao R, Chen Y, Shang MJ, Zhang YH. Primary Hepatic Epithelioid Angiomyolipoma: A Malignant Potential Tumor Which Should Be Recognized. World J Gastroenterol 2016; 22(20): 4908–4917. DOI: 10.3748/wjg.v22.i20.4908.
14. Nguyen TTL, Terris B, Barat M. Hepatic Epithelioid Angiomyolipoma Mimicking Hepatocellular Carcinoma. Diagn Interv Imaging 2020; 101(7–8): 501–503. DOI: 10.1016/j.diii.2020.01.016.
15. Hu WG, Lai EC, Liu H, Li AJ, Zhou WP, Fu SY, Pan ZY, Huang G, Lei Y, Lau WY, Wu MC. Diagnostic Difficulties and Treatment Strategy of Hepatic Angiomyolipoma. Asian J Surg 2011; 34(4): 158–162. DOI: 10.1016/j.asjsur.2011.11.005.
16. Yang J, Zhang HR, Zhang R, Hua X, Cai P, Yan XC. Hepatic Monotypic Epithelioid Angiomyolipoma with Concomitant Hepatocellular Carcinoma. Int J Clin Exp Pathol 2019; 12(4): 1399–1405.
17. Petrolla AA, Xin W. Hepatic Angiomyolipoma. Arch Pathol Lab Med 2008; 132(10): 1679–1682. DOI: 10.5858/2008-132-1679-HA.
18. Zeng JP, Dong JH, Zhang WZ, Wang J, Pang XP. Hepatic Angiomyolipoma: A Clinical Experience in Diagnosis and Treatment. Dig Dis Sci 2010; 55(11): 3235–3240. DOI: 10.1007/s10620-010-1144-2.
19. Wee A. Fine-Needle Aspiration Biopsy of Hepatocellular Carcinoma and Related Hepatocellular Nodular Lesions in Cirrhosis: Controversies, Challenges, and Expectations. Patholog Res Int 2011; 2011: 587936. DOI: 10.4061/2011/587936.
20. Messiaen T, Lefebvre C, Van Beers B, Sempoux C, Cosyns JP, Geubel A. Hepatic Angiomyo(myelo)lipoma: Difficulties in Radiological Diagnosis and Interest of Fine Needle Aspiration Biopsy. Liver 1996; 16(5): 338–341. DOI: 10.1111/j.1600-0676.1996.tb00757.x.
21. Yang L, Xu Z, Dong R, Fan J, Du Y, Zhang Y, Wang X, Cheng X, Guo J. Is Surgery Necessary for Patients with Hepatic Angiomyolipoma? Retrospective Analysis from Eight Chinese Cases. J Gastroenterol Hepatol 2013; 28(10): 1648–1653. DOI: 10.1111/jgh.12289.
22. Chen W, Liu Y, Zhuang Y, Peng J, Huang F, Zhang S. Hepatic Perivascular Epithelioid Cell Neoplasm: A Clinical and Pathological Experience in Diagnosis and Treatment. Mol Clin Oncol 2017; 6(4): 487–493. DOI: 10.3892/mco.2017.1168.
23. Nguyen CL, Nguyen HH, Luong TH, Nguyen NT, Le VK, Vu TK. Giant Hepatic Angiomyolipoma Presenting with Severe Anemia: A Surgical Case Report and Review of Literature. Int J Surg Case Rep 2022; 94: 107087. DOI: 10.1016/j.ijscr.2022.107087.
24. Cai X, Sun S, Deng Y, Liu J, Pan S. Hepatic Epithelioid Angiomyolipoma is Scattered and Unsuitable for Surgery: A Case Report. J Int Med Res 2023; 51(2): 03000605231154657. DOI: 10.1177/03000605231154657.
25. Tajima S, Suzuki A, Suzumura K. Ruptured Hepatic Epithelioid Angiomyolipoma: A Case Report and Literature Review. Case Rep Oncol 2014; 7(2): 369–375. DOI: 10.1159/000363690.