
Acta medica Lituanica ISSN 1392-0138 eISSN 2029-4174
2025. Vol. 32. No 2. Online ahead of print DOI: https://doi.org/10.15388/Amed.2025.32.2.20
Sandeep Yadav
GSVM Medical College, PMSSY Hospital, Kanpur, Uttar-Pradesh, India
E-mail: shintuyadav03@gmail.com
Vrinda
GSVM Medical College, PMSSY Hospital, Kanpur, Uttar-Pradesh, India
E-mail: vrindapaliwal@gmail.com
Pankaj Kumar
School of Health Sciences, Chhatrapati Shahu Ji Maharaj University, Kanpur, Uttar-Pradesh, India
E-mail: pankajkumar@csjmu.ac.in
ORCID ID https://orcid.org/0009-0004-7070-7092
Santosh Kumar Yadav
School of Health Sciences, Chhatrapati Shahu Ji Maharaj University, Kanpur, Uttar-Pradesh, India
E-mail: santosh@csjmu.ac.in
ORCID ID https://orcid.org/0009-0009-1483-9556
Dheeraj Kumar*
School of Health Sciences, Chhatrapati Shahu Ji Maharaj University, Kanpur, Uttar-Pradesh, India
E-mail: dheeraj@csjmu.ac.in
ORCID ID https://orcid.org/0000-0003-4285-8104
Abstract. Neurocysticercosis (NCC), a parasitic infection of the central nervous system caused by Taenia solium larvae, is a leading cause of acquired epilepsy in endemic regions. This case describes a 40-year-old male who presented with chronic headache, dizziness, and a recent seizure episode. He had no prior history of systemic illness, tuberculosis, or neurological disorders. Magnetic Resonance Imaging (MRI) of the brain revealed multiple ring-enhancing lesions with an eccentric scolex in the cerebral and cerebellar hemispheres, accompanied by surrounding edema, confirming the diagnosis of neurocysticercosis. Additional lesions in extraocular, facial, and tongue muscles were consistent with myocysticercosis, an uncommon but clinically significant manifestation that may mimic inflammatory or neoplastic processes.
Spinal imaging demonstrated degenerative changes, including diffuse cervical disc bulges at multiple levels (C3–C7) and lumbar disc pathology at L4–L5, causing anterior thecal sac indentation but without cord compression or myelomalacia. While the spinal findings were incidental, they were clinically relevant as contributors to chronic pain and potential neurological deficits.
The coexistence of disseminated neurocysticercosis with muscular involvement and early degenerative spinal disease highlights the importance of comprehensive evaluation in patients presenting with seizures and persistent headache. Treatment included albendazole-based antiparasitic therapy, corticosteroids to reduce perilesional edema, antiepileptic medications, and conservative management for disc disease.
This case underscores the role of MRI in identifying pathognomonic features of cysticercosis, emphasizes the need for systemic evaluation, and demonstrates the significance of recognizing coexisting pathologies for tailored multidisciplinary management.
Keywords: neurocysticercosis, myocysticercosis, cervical disc disease, lumbar disc pathology, MRI.
Santrauka. Neurocisticerkozė (NCC) – centrinės nervų sistemos parazitinė infekcija, kurią sukelia Taenia solium lervos, yra pagrindinė įgytos epilepsijos priežastis endeminiuose regionuose. Aprašomas 40 metų vyras kreipėsi dėl lėtinio galvos skausmo, galvos svaigimo ir neseniai patirto priepuolio Jis teigė neturėjęs sisteminių ligų, tuberkuliozės ar neurologinių sutrikimų. Magnetinio rezonanso tomografija (MRT) parodė smegenyse esant daugybę žiedinių pažeidimų su skoleksu smegenų ir smegenėlių pusrutuliuose, kartu buvo aplinkinių edemų, patvirtinančių neurocisticerkozės diagnozę. Papildomi pažeidimai akies, veido ir liežuvio raumenyse atitiko raumenų cisticerkozę, retą, bet klinikinę reikšmę turintį simptomą, kuris gali imituoti uždegiminius ar neoplastinius procesus.
Stuburo vaizdinimas parodė degeneracinius pokyčius, įskaitant difuzines kaklo disko išvaržas keliuose lygiuose (C3–C7) ir juosmens disko patologiją L4–L5, sukeliančią priekinio nugaros smegenų maišelio įdubimą, bet be nugaros smegenų suspaudimo ar mielomaliacijos. Nors stuburo radiniai buvo atsitiktiniai, jie klinikiškai reikšmingi kaip prisidedantys prie lėtinio skausmo ir galimų neurologinių sutrikimų.
Kai yra išplitusi neurocisticerkozė kartu su raumenų pažeidimu ir ankstyva degeneracine stuburo liga, ypač svarbu atlikti pacientų, kuriems pasireiškia traukuliai ir nuolatinis galvos skausmas, išsamų vertinimą. Gydant mūsų pacientą taikyta antiparazitinė terapija albendazolo pagrindu, skirta kortikosteroidų edemai mažinti, antiepilepsinių vaistų ir konservatyvus tarplastelinio disko ligos gydymas.
Šis atvejis rodo MRT svarbą nustatant cisticerkozės patognominius požymius, akcentuojama sisteminio vertinimo būtinybė ir kaip svarbu atpažinti kartu pasireiškiančias patologijas, kad būtų galima parinkti individualų daugiadisciplininį gydymą.
Raktažodžiai: neurocisticerkozė, raumenų neurocisticerkozė, tarpslankstelinio disko liga, juosmeninio disko patologija, MRT
_________
* Corresponding author
Received: 18/09/2025. Revised: 09/11/2024. Accepted: 27/11/2025
Copyright © 2025 Sandeep Yadav, Vrinda, Pankaj Kumar, Santosh Kumar Yadav, Dheeraj Kumar. Published by Vilnius University Press.This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Neurocysticercosis (NCC) is a parasitic infection of the central nervous system caused by the larval form of Taenia solium. It is one of the leading causes of acquired epilepsy in developing countries and continues to be a major public health concern in India and other endemic regions [1]. The disease can affect the brain, spinal cord, and sometimes skeletal muscles, producing a wide range of neurological symptoms depending on the number and location of cysts.
Magnetic Resonance Imaging (MRI) remains the most sensitive imaging tool for detecting the characteristic features of NCC, including ring-enhancing cystic lesions with an eccentric scolex and perilesional edema [2]. It also assists in distinguishing NCC from other intracranial pathologies such as tuberculoma, abscess, or metastasis [3]. The present case report highlights a 40-year-old male with disseminated neurocysticercosis and coexisting cervical and lumbar disc pathology. It emphasizes the diagnostic value of MRI in identifying both parasitic and degenerative changes and underlines the importance of a multidisciplinary approach for accurate diagnosis and comprehensive management.
A 40-year-old male presented to the neurology clinic with complaints of persistent headache for approximately six months and recurrent dizziness for the past three months. He also experienced a generalized seizure episode on 18 April 2025, which prompted detailed neurological evaluation. The patient had no prior history of systemic illness, tuberculosis, head trauma, or familial neurological disorders. On examination, he was conscious and oriented, with no focal neurological deficit.
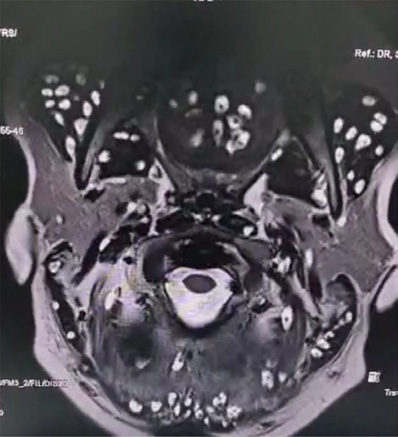
Magnetic Resonance Imaging (MRI) of the brain demonstrated multiple well-defined ring-enhancing lesions with eccentric mural nodules representing the scolex in the bilateral cerebral and cerebellar hemispheres, accompanied by surrounding edema – which are findings highly suggestive of neurocysticercosis (Figure 1) [4].

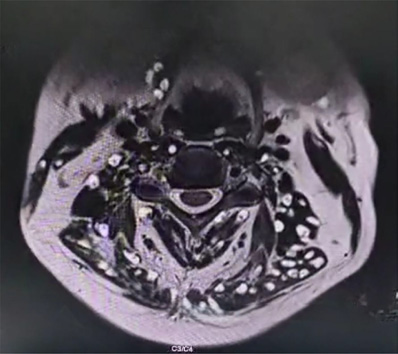
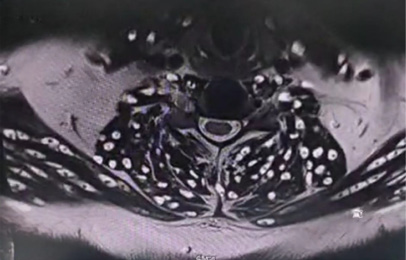
In addition, multiple cystic lesions were observed within the extraocular, facial, and tongue muscles, each containing an eccentric scolex, consistent with disseminated myocysticercosis (Figures 2 and 3). These lesions exhibited hyperintense signals on T2-weighted and hypointense signals on T1-weighted sequences, confirming their parasitic nature.
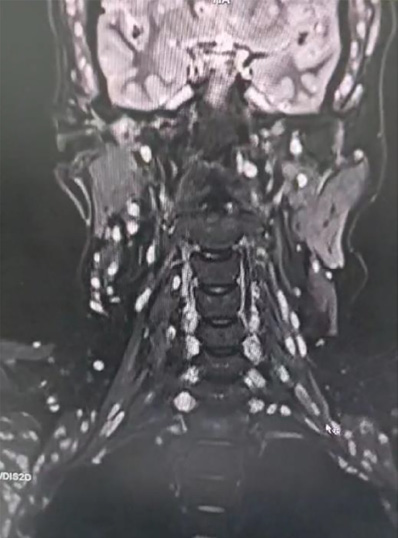
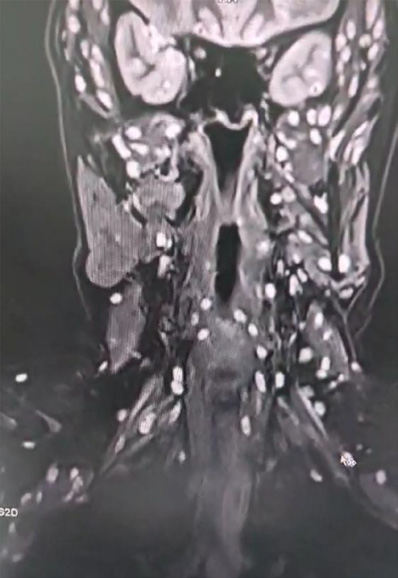
Spinal MRI revealed reversal of cervical lordosis with diffuse disc bulges at levels C3/4, C4/5, C5/6, and C6/7, causing mild anterior thecal-sac indentation but without evidence of cord compression or myelomalacia (Figures 4–7) [5]. The lumbar spine showed disc desiccation with a diffuse bulge at L4–L5, indenting the thecal sac yet preserving normal vertebral body height and marrow signal intensity. No paravertebral abscess, vertebral destruction, or compressive myelopathy was noted [6].

Based on these findings, a final diagnosis of disseminated neurocysticercosis with muscular involvement and coexisting cervical and lumbar degenerative disc disease was made. The patient was treated with albendazole (15 mg/kg/day) and oral corticosteroids to reduce perilesional edema, along with antiepileptic therapy for seizure control. For spinal symptoms, conservative management with analgesics and physiotherapy was advised [7].
Neurocysticercosis as a common cause of seizures – in endemic regions, NCC should be suspected in patients presenting with new-onset seizures and chronic headache. Recognition of the scolex within cystic lesions on MRI is pathognomonic and crucial for diagnosis. Muscular cysticercosis, though uncommon, may present in extraocular, facial, and tongue muscles. Identifying the scolex differentiates it from abscesses or neoplastic lesions, preventing unnecessary invasive procedures. MRI remains the gold standard for detecting CNS and muscular involvement, delineating active disease, and excluding differential diagnoses such as tuberculomas or metastases [8]. Degenerative disc bulges, though incidental, may contribute to chronic pain or radiculopathy. Their recognition prevents misattribution of neurological symptoms solely to NCC. Optimal care requires antiparasitic therapy, seizure control, corticosteroids, and orthopedic/rehabilitative support for spinal degeneration.
Neurocysticercosis with Myocysticercosis was diagnosed.
This case report represents a single-patient observation; therefore, the findings cannot be generalized to a larger population. The diagnosis was based on characteristic MRI features without histopathological confirmation. Additionally, long-term follow-up imaging was not available to evaluate treatment response. Despite these constraints, the case provides valuable clinical and radiological insights into the coexistence of disseminated neurocysticercosis and degenerative spinal disease.
Q1. What are the characteristic MRI findings that confirm neurocysticercosis?
Explanation: On MRI, neurocysticercosis is identified by multiple ring-shaped lesions, each showing an eccentric nodule representing the scolex. These lesions are often accompanied by perilesional edema. In this case, their presence in the cerebral and cerebellar hemispheres provided a clear and definitive diagnosis.
Q2. How is muscular (myocysticercosis) involvement identified in this patient?
Explanation: Muscular involvement was detected through MRI, which revealed multiple cystic lesions within the extraocular, facial, and tongue muscles. The presence of an eccentric scolex inside these lesions confirmed that they were parasitic in origin, indicating disseminated myocysticercosis, which is an uncommon but clinically relevant finding.
Q3. What was the significance of the cervical and lumbar disc pathology?
Explanation: Imaging showed diffuse disc bulges at multiple cervical levels (C3–C7) and at the lumbar level (L4–L5). These changes caused indentation of the anterior thecal sac, consistent with early degenerative disc disease. Although unrelated to the parasitic infection, these findings explained the patient’s chronic pain and required attention to avoid future complications.
Q4. What was the multidisciplinary management approach for this patient?
Explanation: The patient was started on albendazole to target the parasitic infection, with corticosteroids prescribed to reduce associated inflammation and edema. Antiepileptic medication was given to control seizures. For spinal disc disease, a conservative plan including analgesics and physiotherapy was advised. This combined approach emphasized the importance of collaboration between neurology, infectious disease, and orthopedics in achieving optimal patient outcomes.
All authors were actively involved in conceptualizing the paper, conducting the case research, and preparing as well as editing the manuscript.
S.Y.: Investigation, Methodology, Writing – Original Draft.
V.: Data Curation, Formal Analysis, Writing – Review and Editing.
P.K.: Resources, Visualization, Literature Review.
S.K.Y.: Validation, Writing – Review and Editing.
D.K.: Project Administration, Final Editing, Correspondence, Overall Supervision.
The authors express their sincere gratitude to the radiology department and all of its staff for their valuable guidance and continuous support throughout the preparation and publication of this case report.
The authors declare that there are no conflicts of interest involved in this research or financial disclosures related to this case report.
Patient consent was not required as no identifiable personal information is included in this report.
This study did not involve any human or animal experiments.